Types of Diabetes
Type 1 Diabetes






Type 2 Diabetes




Type 3 Diabetes
Gestational Diabetes

Symptoms and Complications
Symptoms

Complications

Understanding Diabetes: A Guide to Managing and Curing Your Diabetes
Understanding Diabetes is crucial for managing and preventing complications. This article provides an overview of diabetes, including its types, symptoms, and impact on health. It also covers the importance of early recognition, management strategies, and the role of lifestyle changes. Additionally, it explores gestational diabetes, prediabetes, and diabetes complications, along with medical management options. The article emphasizes the significance of maintaining a healthy lifestyle, seeking support, and staying informed. Explore the topics and resources to gain a better understanding of diabetes and its management.
Understanding Diabetes: An Overview
Welcome to the comprehensive overview of diabetes. In this section, we will delve into the key aspects of this chronic condition, without getting into the specific details mentioned in later sections. It is crucial to understand what diabetes is, why it is important to grasp its nature, and the impact it can have on our health.
What is Diabetes?
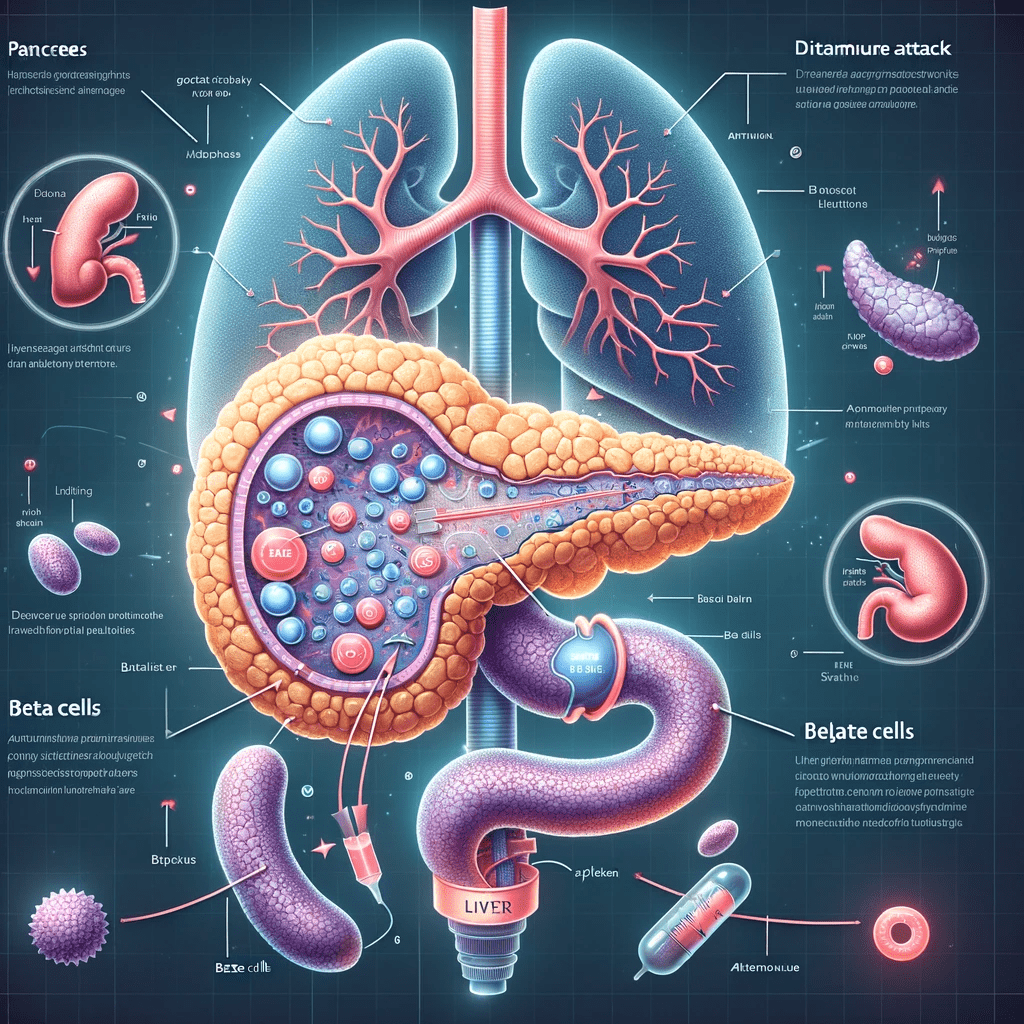
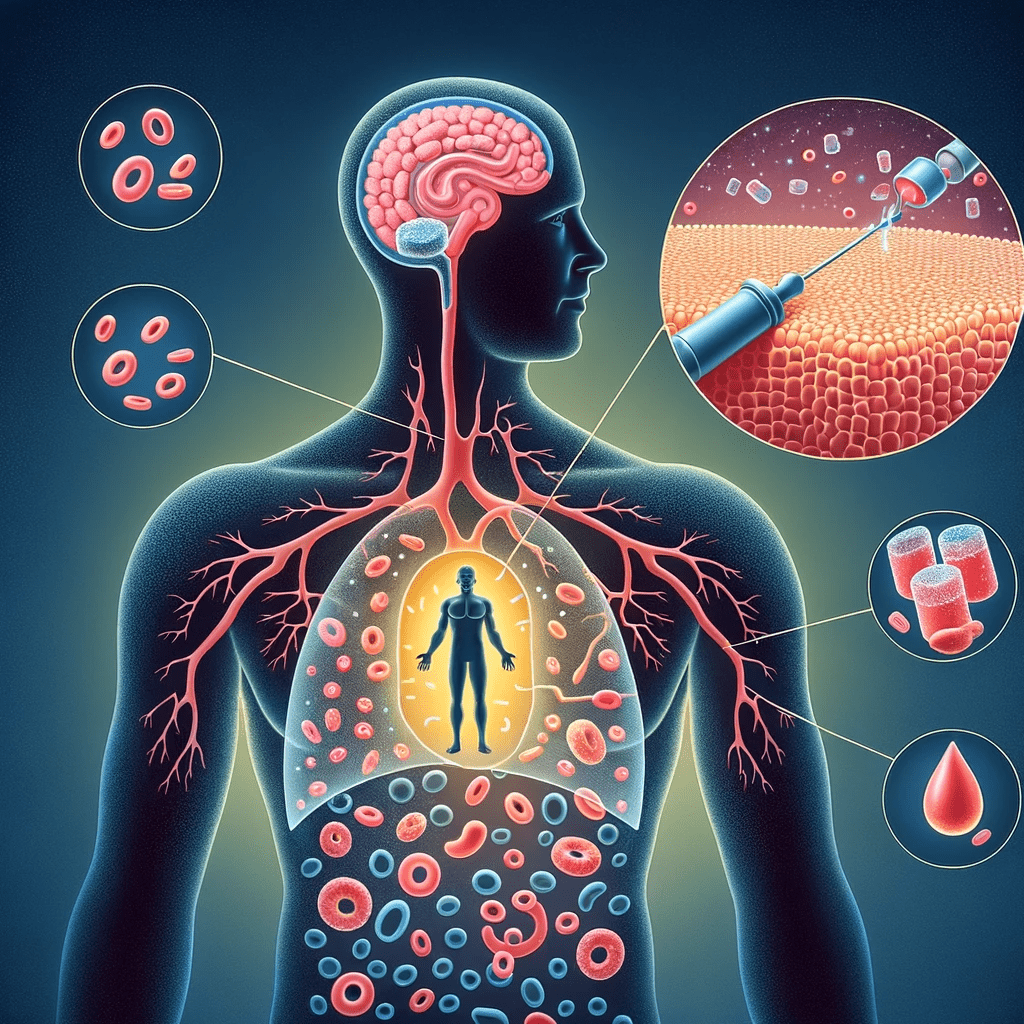
Diabetes is a chronic disease that affects the body's ability to convert food into energy. It is characterized by either a deficiency in insulin production or the body's inadequate response to insulin. Insulin is a hormone produced by the pancreas to regulate blood sugar levels. When we consume food, it breaks down into glucose, which enters the bloodstream. Insulin helps glucose enter cells for energy utilization. However, in diabetes, this process is impaired, leading to elevated blood sugar levels.
Why is Understanding Diabetes Important?
Having a comprehensive understanding of diabetes is crucial for several reasons. Firstly, it allows individuals to recognize the symptoms and seek timely medical intervention. Early diagnosis and management significantly reduce the risk of long-term complications. Secondly, understanding diabetes empowers individuals to make informed lifestyle choices. A well-rounded knowledge enables the implementation of appropriate dietary changes, regular physical activity, and stress management techniques. Lastly, awareness of diabetes promotes empathy and support for those living with the condition, fostering a supportive community.
The Impact of Diabetes on Health
Diabetes has a significant impact on health, affecting various body systems and increasing the risk of complications. Uncontrolled diabetes can lead to cardiovascular diseases such as heart attack and stroke. It also impairs the function of organs like the kidneys, leading to chronic kidney disease. Diabetes can cause nerve damage (neuropathy), affecting sensation and causing complications in the feet and hands. Additionally, it can negatively impact vision, oral health, and mental well-being. Understanding the potential health risks associated with diabetes emphasizes the importance of disease management and prevention.
Recognizing Diabetes Symptoms
Recognizing diabetes symptoms is crucial for early detection and timely intervention. Being aware of the common signs and symptoms can help individuals identify potential risks and seek appropriate medical advice.
Common Symptoms of Diabetes
- Frequent urination
- Increased thirst
- Unexplained weight loss
- Extreme hunger
- Fatigue and tiredness
- Blurred vision
- Slow-healing sores
- Recurrent infections
Experiencing these symptoms may indicate the presence of diabetes and warrant a visit to a healthcare professional for further evaluation.
Early Warning Signs of Type 1 Diabetes
Type 1 diabetes tends to manifest with sudden and noticeable symptoms. Some early warning signs to watch out for include:
- Increased thirst and frequent urination
- Unexplained weight loss despite increased appetite
- Constant fatigue and weakness
- Irritability and mood changes
If these symptoms are observed, especially in children or young adults, it is essential to seek medical attention promptly.
Signs and Symptoms of Type 2 Diabetes
Type 2 diabetes symptoms can develop gradually and may be less apparent initially. However, being vigilant about the following signs can facilitate early diagnosis:
- Increased thirst and dry mouth
- Frequent urination, particularly at night
- Fatigue and tiredness despite adequate rest
- Blurry vision
- Skin infections and slow-healing wounds
- Tingling or numbness in the hands or feet
If any of these symptoms are present, it is important to consult a healthcare professional for a comprehensive evaluation and appropriate management.
Understanding Type 1 Diabetes
Welcome to the section on understanding type 1 diabetes. In this section, we will explore the causes, risk factors, diagnosis, management, challenges, and coping strategies associated with type 1 diabetes.
Causes and Risk Factors of Type 1 Diabetes
Type 1 diabetes is believed to be caused by an autoimmune reaction in which the body's immune system attacks and destroys the insulin-producing cells in the pancreas. While the exact cause is unknown, genetic and environmental factors play a role in the development of type 1 diabetes. Certain genes and viral infections have been linked to the risk of developing this form of diabetes.
Diagnosing and Managing Type 1 Diabetes
Diagnosing type 1 diabetes involves various blood tests to measure blood sugar levels and determine the presence of specific antibodies. Once diagnosed, individuals with type 1 diabetes require insulin therapy to regulate their blood sugar levels. Monitoring blood glucose levels, administering insulin, and managing carbohydrate intake are key aspects of managing type 1 diabetes. Regular medical check-ups and consultations with a healthcare team are crucial for proper management.
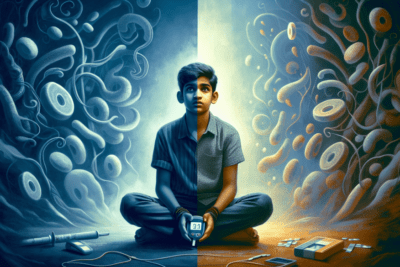
Living with Type 1 Diabetes: Challenges and Coping Strategies
Living with type 1 diabetes presents unique challenges. The need for regular blood sugar monitoring, insulin administration, and adhering to a strict dietary and exercise routine can be overwhelming. Additionally, managing diabetes while engaging in everyday activities, such as school, work, and social events, requires careful planning.
To cope with these challenges, it is important to build a strong support system and develop effective coping strategies. Seeking support from healthcare professionals, connecting with others who have type 1 diabetes, and staying informed about the latest advancements in diabetes management can make a significant difference in navigating the daily challenges of living with type 1 diabetes.
While living with type 1 diabetes requires diligence and adjustment, it is possible to lead a fulfilling life by effectively managing the condition and staying proactive in one's self-care routine.
Understanding Type 2 Diabetes
Understanding type 2 diabetes is crucial for effective management and prevention of complications. This section explores the causes and risk factors of type 2 diabetes, as well as strategies for prevention and management, including lifestyle changes for better control.
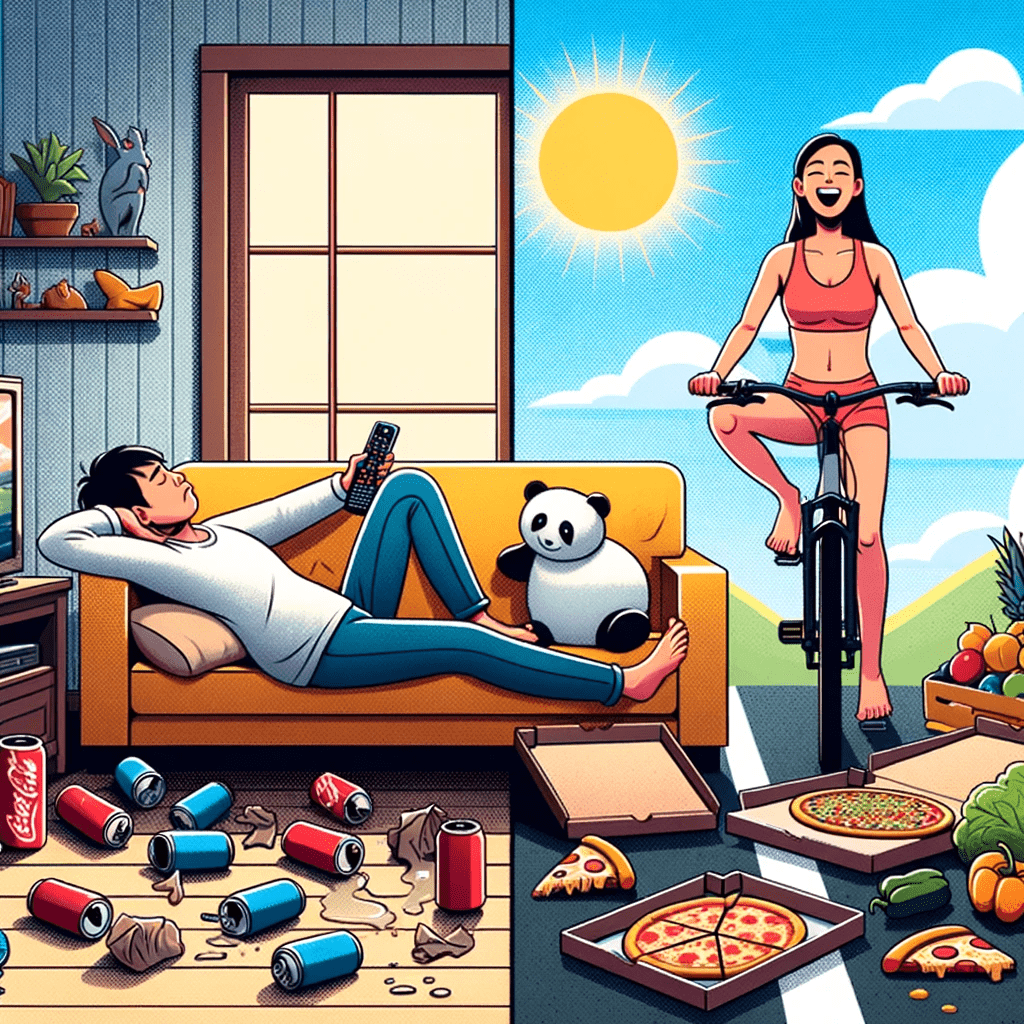
Causes and Risk Factors of Type 2 Diabetes
Type 2 diabetes is primarily characterized by insulin resistance and inadequate insulin production. While the exact causes are still being studied, several risk factors can contribute to the development of type 2 diabetes:
- Obesity or overweight
- Inactivity or sedentary lifestyle
- Unhealthy eating habits, particularly consuming processed foods and sugary beverages
- Family history of diabetes
- High blood pressure
- Elevated cholesterol levels
- Having prediabetes
- Age (being over 45 years old)
- Certain ethnicities, such as African American, Hispanic, Asian, and Native American
It's important to note that having one or more risk factors doesn't necessarily mean one will develop type 2 diabetes. However, it's advisable to be aware of these factors and make proactive lifestyle choices to mitigate the risk.
Prevention and Management of Type 2 Diabetes
The good news is that type 2 diabetes can often be prevented or delayed through certain lifestyle modifications. By adopting the following strategies, individuals can significantly reduce their risk:
- Maintaining a healthy weight: Losing excess weight and maintaining a healthy BMI can be beneficial in preventing the onset of type 2 diabetes.
- Regular physical activity: Engaging in regular exercise, such as brisk walking, swimming, or cycling, helps improve insulin sensitivity and manage blood sugar levels.
- Healthy eating habits: Opting for a nutritious, balanced diet that includes whole grains, lean proteins, fruits, vegetables, and healthy fats can contribute to diabetes prevention.
- Limiting sugary and processed foods: Minimizing the consumption of sugary beverages, desserts, and highly processed foods can help control blood sugar levels and reduce the risk of diabetes.
- Quitting smoking: Smoking increases the risk of various health conditions, including type 2 diabetes. Quitting smoking can significantly improve overall health.
Lifestyle Changes for Type 2 Diabetes Control
For individuals already living with type 2 diabetes, making certain lifestyle changes can play a vital role in managing the condition effectively:
- Regular monitoring of blood sugar levels: Checking blood sugar levels at home using a glucometer helps individuals with diabetes stay aware of their current levels and make necessary adjustments.
- Meal planning and portion control: Following a structured meal plan that includes a balanced mix of carbohydrates, proteins, and fats, along with portion control, can help stabilize blood sugar levels.
- Regular physical activity: Engaging in regular exercise promotes weight management, improves insulin sensitivity, and contributes to overall well-being.
- Stress management: Finding healthy ways to cope with stress, such as practicing mindfulness, deep breathing, or engaging in hobbies, can positively impact diabetes management.
- Medication adherence: Following the prescribed medication regimen as instructed by healthcare professionals is crucial for maintaining proper blood sugar control.
By implementing these lifestyle changes, individuals with type 2 diabetes can improve their overall health and reduce the risk of complications associated with the condition.
Gestational Diabetes: Risks and Management
Gestational diabetes is a temporary form of diabetes that affects pregnant women. It is characterized by high blood sugar levels that can pose risks to both the mother and the baby. Understanding the risks and effectively managing gestational diabetes during pregnancy is crucial for a healthy outcome.
What is Gestational Diabetes?
Gestational diabetes occurs when hormone changes during pregnancy cause insulin resistance, leading to high blood sugar levels. This condition typically develops around the 24th to 28th week of pregnancy and affects about 7% of pregnant women in the United States.
Managing Gestational Diabetes during Pregnancy
The primary goals of managing gestational diabetes are to keep blood sugar levels within a target range and ensure the well-being of both the mother and the baby. This often involves lifestyle changes, such as adopting a healthy eating plan, engaging in regular physical activity, and monitoring blood sugar levels. In some cases, medication or insulin may be necessary to control blood sugar levels effectively.
Regular prenatal check-ups and working closely with a healthcare team are vital for managing gestational diabetes. Monitoring blood sugar levels, adhering to a recommended meal plan, and maintaining a regular exercise routine are essential components of effective management.
Long-term Effects and Prevention of Gestational Diabetes
While gestational diabetes usually resolves after giving birth, women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life. It is crucial to monitor blood sugar levels after delivery and make lifestyle modifications to reduce the risk of developing diabetes in the future.
Furthermore, women who have experienced gestational diabetes should inform their healthcare providers about their medical history when planning future pregnancies. Managing weight, adopting healthy habits, and seeking regular medical check-ups can help prevent or mitigate the risks associated with gestational diabetes in subsequent pregnancies.
By understanding the risks associated with gestational diabetes and actively managing the condition during pregnancy, women can optimize their health and that of their babies. Close monitoring and a proactive approach to postpartum care can play a significant role in preventing long-term health complications.
Prediabetes: Understanding the Warning Signs
Prediabetes refers to a condition in which blood sugar levels are higher than normal but not yet high enough to be diagnosed as type 2 diabetes. It serves as a crucial warning sign, indicating an increased risk of developing diabetes in the future. Understanding the warning signs and taking appropriate action can help prevent the progression to full-blown diabetes.
What is Prediabetes?
Prediabetes is a metabolic condition that occurs when the body's cells become resistant to the effects of insulin, leading to elevated blood sugar levels. It is often considered a precursor to type 2 diabetes, but it's important to note that not everyone with prediabetes will develop diabetes. With the right lifestyle modifications, prediabetes can be reversed, and the risk of developing diabetes can be greatly reduced.
Risk Factors and Prevention of Prediabetes
Several risk factors contribute to the development of prediabetes, including being overweight or obese, having a sedentary lifestyle, having a family history of diabetes, and being over the age of 45. Certain ethnicities, such as African Americans, Hispanics, and Asians, also have a higher predisposition to prediabetes.
To prevent prediabetes and reduce the risk of developing diabetes, lifestyle modifications play a crucial role. Incorporating regular physical activity, aiming for a healthy weight, and adopting a balanced diet that includes fruits, vegetables, whole grains, lean proteins, and healthy fats can significantly reduce the chances of progression to diabetes.
Strategies for Reversing Prediabetes and Preventing Diabetes
Reversing prediabetes requires comprehensive lifestyle changes. This includes engaging in moderate-intensity aerobic exercise for at least 150 minutes per week, along with strength training activities twice a week. Making dietary adjustments, such as reducing the consumption of sugary beverages and processed foods, can also contribute to improved blood sugar control.
In addition, weight loss is often recommended for individuals with prediabetes. Losing as little as 5-7% of body weight can have a significant impact on blood sugar levels and reduce the risk of developing diabetes. Monitoring blood glucose levels regularly and seeking support from healthcare professionals or diabetes education programs can provide invaluable guidance and encouragement throughout the journey.
- Engage in moderate-intensity aerobic exercise for at least 150 minutes per week
- Incorporate strength training activities twice a week
- Opt for a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
- Reduce the consumption of sugary beverages and processed foods
- Aim for gradual and sustainable weight loss (5-7% of body weight)
- Monitor blood glucose levels regularly
- Seek support from healthcare professionals or diabetes education programs
By taking proactive steps to address prediabetes, individuals can significantly lower their risk of developing type 2 diabetes and improve their overall health and well-being.
Diabetes Complications and Their Prevention
Impact of Diabetes on Kidney Health
Diabetes can have a significant impact on kidney health, increasing the risk of developing chronic kidney disease. High blood sugar levels over time can damage the kidneys' tiny blood vessels and impair their ability to filter waste and excess fluids from the body. To prevent complications, it is crucial for individuals with diabetes to control their blood sugar levels, maintain healthy blood pressure, and undergo regular kidney function tests.
Heart Disease and Diabetes: Managing the Risk
Heart disease is a major concern for individuals with diabetes, as they have a higher risk of developing cardiovascular problems. Diabetes can contribute to the buildup of plaque in the arteries, increasing the likelihood of heart attacks and strokes. Managing diabetes and reducing risk factors such as high blood pressure, high cholesterol, and smoking is essential in preventing heart disease. Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, and medication if necessary, can help individuals with diabetes maintain optimal heart health.
Eye and Foot Health in Diabetes
Diabetes can also impact eye and foot health, leading to complications such as diabetic retinopathy and diabetic neuropathy. Diabetic retinopathy occurs when high blood sugar levels damage the blood vessels in the retina, potentially leading to vision loss. Regular eye examinations and proper blood sugar control are vital for preserving vision. Diabetic neuropathy affects the nerves in the feet, making it crucial to take preventive measures to avoid foot ulcers and infections. Regular foot inspections, proper foot hygiene, wearing well-fitting shoes, and managing blood sugar levels are essential for maintaining foot health.
Understanding and actively addressing diabetes complications is crucial for individuals with diabetes. By closely managing blood sugar levels, adopting a healthy lifestyle, regularly monitoring their health, and seeking appropriate medical care, individuals can significantly reduce the risk and severity of complications related to diabetes.
Medical Management of Diabetes
Medical management plays a crucial role in effectively controlling diabetes. It involves various components such as understanding insulin, the use of oral medications, and monitoring blood sugar levels through A1C testing.
Understanding Insulin and Its Importance
Insulin is a hormone produced by the pancreas that regulates blood sugar levels. For individuals with diabetes, understanding insulin and its role is paramount. Insulin can be delivered through injections or the use of an insulin pump. It helps to move glucose from the bloodstream into cells, where it is used for energy. Different types of insulin are available, including fast-acting, short-acting, intermediate-acting, and long-acting insulin. The type and dosage of insulin required vary depending on individual needs, and healthcare professionals guide patients in adjusting their insulin regimen as necessary.
Oral Medications for Diabetes Control
In addition to insulin therapy, oral medications are available for managing diabetes, especially in cases of type 2 diabetes. These medications work in various ways to help control blood sugar levels. Some help the pancreas produce more insulin, while others improve insulin sensitivity or reduce glucose production in the liver. Healthcare providers prescribe oral medications based on an individual's specific needs, medical history, and response to the medication. It is crucial to follow the prescribed dosage and discuss any concerns or potential side effects with a healthcare professional.
Blood Sugar Monitoring and A1C Testing
Monitoring blood sugar levels is vital for diabetes management. Regular testing provides valuable information on how well blood sugar is controlled and helps adjust treatment plans as needed. Self-monitoring of blood glucose levels is often done with a handheld blood glucose meter, which requires a small blood sample obtained through a fingerstick. Another valuable tool is the A1C test, which measures the average blood sugar levels over the past two to three months. This test provides a broader perspective on overall diabetes management and helps healthcare professionals make informed decisions regarding treatment adjustments.
By understanding insulin, utilizing oral medications, and monitoring blood sugar levels through A1C testing, individuals with diabetes can effectively manage their condition and reduce the risk of complications. Regular communication with healthcare professionals, adherence to prescribed medications and testing protocols, and proactive engagement in self-care are all essential aspects of medical management for optimal diabetes control.
Living a Healthy Life with Diabetes
Living a healthy life with diabetes is crucial for effectively managing the condition and minimizing the risk of complications. This section will cover key aspects of diabetes management, including healthy eating, exercise, and mental health.
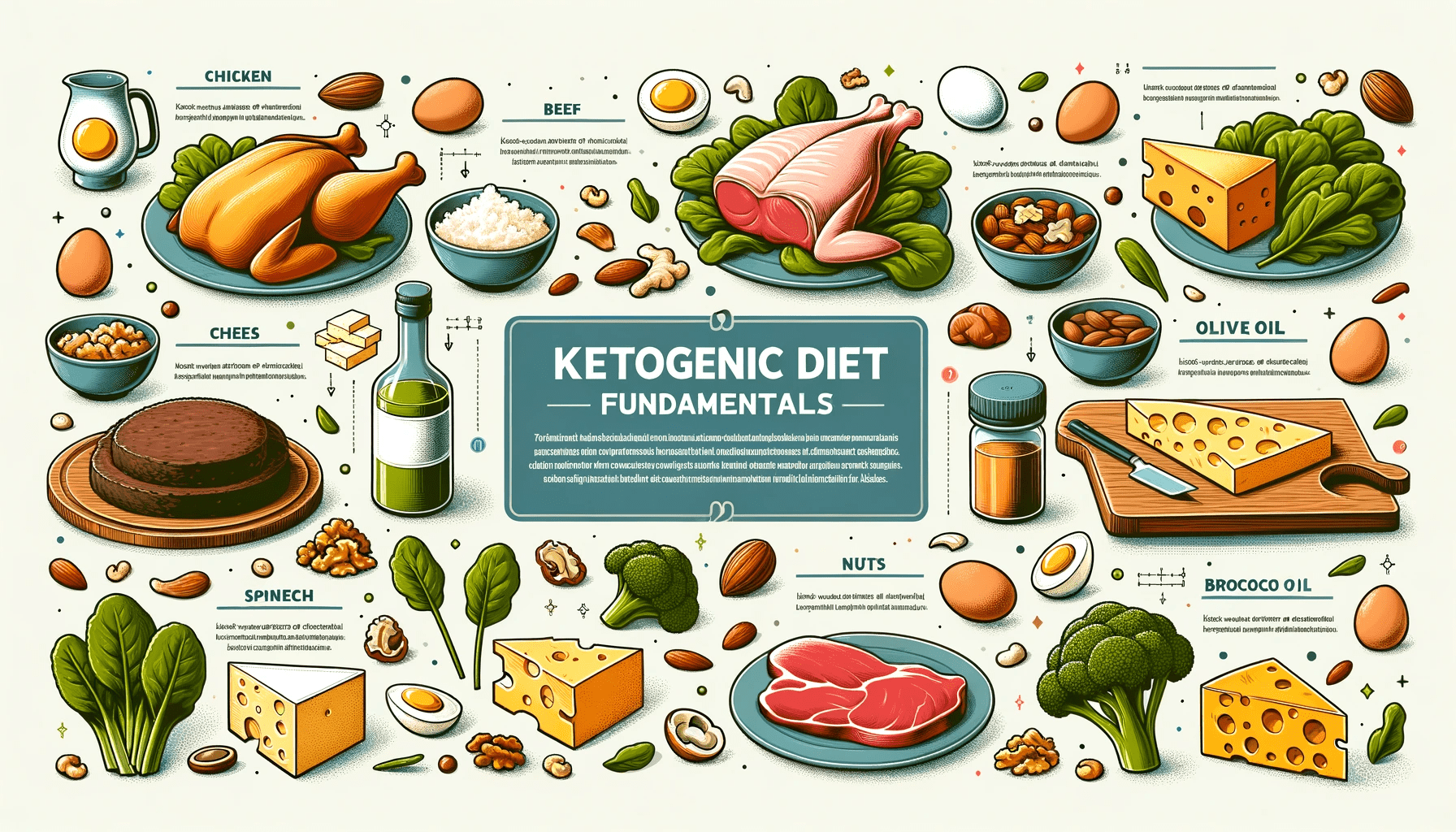
Diabetes Management through Healthy Eating
Proper nutrition plays a vital role in diabetes management. By making healthy food choices, you can control your blood sugar levels and maintain overall well-being. Focus on a balanced diet that includes a variety of nutrient-rich foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of sugary and processed foods, as they can cause sharp spikes in blood sugar. It is also essential to monitor portion sizes and spread your meals evenly throughout the day to prevent blood sugar fluctuations.
The Role of Exercise in Diabetes Control
Regular physical activity offers numerous benefits for individuals with diabetes. Engaging in exercise helps improve insulin sensitivity, lowers blood sugar levels, aids in weight management, and promotes cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic activity, such as brisk walking, cycling, or swimming, spread across the week. Additionally, incorporate strength training exercises to build muscle and boost metabolism. Remember to consult with your healthcare team before starting any exercise program and monitor your blood sugar levels during activity.
Mental Health and Emotional Well-being with Diabetes
Living with diabetes can sometimes take a toll on your mental health and emotional well-being. It is essential to prioritize self-care and seek support when needed. Manage stress through relaxation techniques, such as deep breathing, meditation, or yoga. Maintain a strong support system by connecting with family, friends, or diabetes support groups who can provide understanding and encouragement. If you experience persistent feelings of anxiety, depression, or distress, consider reaching out to a mental health professional for additional assistance. Remember that taking care of your mental health is just as important as managing your physical health when it comes to living well with diabetes.
Diabetes Research and the Latest Advances
Research plays a crucial role in advancing our understanding of diabetes and developing innovative treatments. Ongoing studies focus on various aspects of diabetes to improve management and find potential cures. Here are key subtopics in diabetes research:
Ongoing Research in Diabetes Treatment
Scientists and medical professionals continue to explore new avenues for treating diabetes. Ongoing research efforts include:
- Investigating the effectiveness of new medications in managing blood sugar levels.
- Developing advanced insulin delivery methods to enhance the convenience and effectiveness of insulin therapy.
- Exploring the potential of islet cell transplantation as a treatment option for type 1 diabetes.
- Studying bariatric surgery's impact on diabetes management and remission.
- Investigating the role of gut microbiota in diabetes development and potential interventions.
Promising Advances and Future Directions
Exciting advancements in diabetes research hold promise for improving patient outcomes and quality of life. Some of these include:
- Development of artificial pancreas systems that automate insulin administration based on continuous glucose monitoring.
- Advances in stem cell research to regenerate insulin-producing cells and potentially cure type 1 diabetes.
- Exploration of personalized medicine approaches to optimize diabetes management based on individual genetic and metabolic profiles.
- Investigation of novel therapies targeting inflammation and insulin resistance in type 2 diabetes.
Resources for Staying Informed about Diabetes
To stay up to date with the latest advancements in diabetes research, various resources are available:
- Leading medical journals, such as Diabetes Care, Diabetes, and The Journal of Clinical Endocrinology & Metabolism, publish cutting-edge research on diabetes.
- Participating in clinical trials can provide access to innovative treatments and contribute to the advancement of diabetes research.
- Attending diabetes conferences and seminars allows healthcare professionals and individuals with diabetes to network and learn from experts in the field.
- Non-profit organizations like the American Diabetes Association and the Juvenile Diabetes Research Foundation (JDRF) provide resources and updates on the latest research findings.
Staying informed about diabetes research is crucial for individuals with diabetes, healthcare providers, and researchers alike. Continual advancements in our understanding of diabetes offer hope for improved treatments, better management strategies, and ultimately, the potential for a cure.
Frequently Asked Questions about Diabetes
Here, we address common questions and concerns about diabetes to provide clarity and dispel misconceptions.
Answers to Common Questions about Diabetes
- Q: What are the different types of diabetes?
- Q: Can diabetes be prevented?
- Q: What are the symptoms of diabetes?
- Q: Is diabetes hereditary?
- Q: How is diabetes diagnosed?
Addressing Concerns and Misconceptions
- Q: Can diabetes only affect older people?
- Q: Will I need insulin if I have type 2 diabetes?
- Q: Can I still eat sweets if I have diabetes?
- Q: Does taking insulin mean my diabetes is getting worse?
- Q: Can diabetes be cured?
It is important to consult with a healthcare professional for personalized advice and to address any specific concerns or questions about diabetes.
Seeking Support and Diabetes Care
Building a Diabetes Care Team
Managing diabetes requires a collaborative approach involving a dedicated diabetes care team. This team typically includes healthcare professionals such as endocrinologists, certified diabetes educators, dietitians, and nurses who specialize in diabetes care. Building a strong diabetes care team is essential for receiving comprehensive and personalized care.
Finding Local Resources and Support Groups
Locating local resources and support groups can provide valuable support and guidance throughout your diabetes journey. Check with your healthcare provider, local hospitals, or community centers for diabetes education programs, workshops, and support groups. These resources can offer education, emotional support, and practical advice on managing diabetes effectively.
Local Resources:
- Diabetes education programs
- Workshops on nutrition and meal planning
- Exercise classes for individuals with diabetes
- Support groups for emotional support
Empowering Yourself in Diabetes Management
Empowering yourself in diabetes management involves taking an active role in your own care. This includes learning about diabetes, keeping up with the latest research, and staying informed about treatment options. With knowledge comes empowerment, allowing you to make informed decisions and effectively manage your diabetes.
Key steps to self-empowerment in diabetes management:
- Continuously educate yourself about diabetes through reliable sources.
- Stay updated on the latest research and treatment advancements.
- Take an active role in your treatment plan and engage in open communication with your healthcare team.
- Set realistic goals and track your progress towards achieving them.
- Make healthy lifestyle choices, including a balanced diet, regular physical activity, stress management, and adequate sleep.
- Find coping strategies to deal with the emotional challenges that may come with living with diabetes.
- Surround yourself with a supportive network of family, friends, and peer support groups.
✨ Other articles you might be interested in:
