How to Cure Diabetes Type 2 Permanently: Complete Guide

Diabetes Type 2 can have long-term effects on your health. Understanding the condition is crucial to finding effective treatment options. This article provides an overview of what Diabetes Type 2 is and its causes, symptoms, and diagnosis. It also explores various treatment methods, including medication, diet, exercise, and lifestyle changes. Additionally, we'll discuss achieving diabetes remission through weight loss and bariatric surgery. Managing blood sugar levels and self-care tips will be offered, along with helpful resources and support for living with Diabetes Type 2. How to Cure Diabetes Type 2 Permanently: Complete Guide
- Understanding Diabetes Type 2 - How to Cure Diabetes Type 2 Permanently: Complete Guide
- Diabetes Type 2 Treatment Options - How to Cure Diabetes Type 2 Permanently: Complete Guide
- Achieving Diabetes Remission - How to Cure Diabetes Type 2 Permanently: Complete Guide
- Managing Diabetes Type 2 - How to Cure Diabetes Type 2 Permanently: Complete Guide
- Diabetes Type 2 Resources and Support - How to Cure Diabetes Type 2 Permanently: Complete Guide
Understanding Diabetes Type 2 - How to Cure Diabetes Type 2 Permanently: Complete Guide
What is Diabetes Type 2?
Diabetes Type 2, also known as adult-onset diabetes, is a chronic metabolic disorder characterized by high blood sugar levels. Unlike Type 1 Diabetes, which is an autoimmune disease, Type 2 Diabetes occurs when the body becomes resistant to insulin or doesn't produce enough insulin to regulate blood sugar effectively. Insulin is a hormone that helps glucose enter cells to provide energy. Without proper regulation, high blood sugar levels can lead to various complications over time.
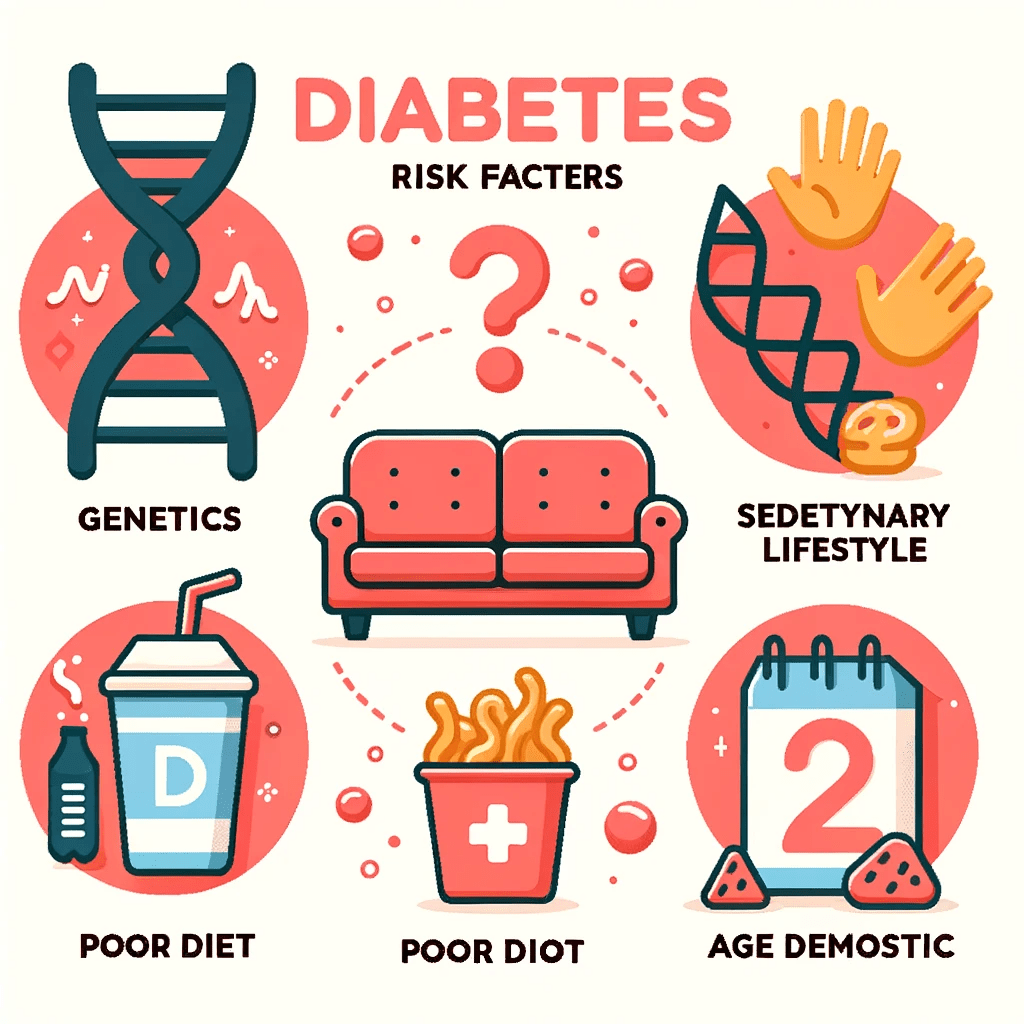
Causes and Risk Factors
The exact cause of Type 2 Diabetes is not fully understood, but various factors contribute to its development. These include genetics, lifestyle choices, and certain health conditions. People with a family history of Type 2 Diabetes are at higher risk, as genetics can influence insulin resistance. Additionally, sedentary lifestyles, poor diet choices, obesity, and age above 45 are associated with an increased risk of developing Type 2 Diabetes. Certain ethnicities, such as African Americans, Hispanic Americans, and Native Americans, also have a higher predisposition to the condition.
Symptoms and Diagnosis
Early stages of Type 2 Diabetes may not exhibit noticeable symptoms. However, as the condition progresses, individuals may experience frequent urination, increased thirst, unexplained weight loss, fatigue, blurred vision, slow wound healing, and recurrent infections. If these symptoms are present, it is important to consult a healthcare professional for diagnosis. Diagnosis typically involves a series of blood tests, including fasting blood sugar tests, oral glucose tolerance tests, and glycated hemoglobin (A1C) tests, which provide insights into blood sugar levels over time.
Understanding Diabetes Type 2 is crucial for effective management and exploring treatment options. By recognizing the causes, risk factors, symptoms, and diagnostic processes related to this condition, individuals can take proactive steps towards optimizing their health and well-being.
Diabetes Type 2 Treatment Options - How to Cure Diabetes Type 2 Permanently: Complete Guide
Managing diabetes type 2 involves a combination of medication, diet and nutrition, and regular physical activity. A comprehensive treatment plan can help control blood sugar levels, reduce complications, and improve overall health.
Medication and Insulin
Medication plays a crucial role in the treatment of diabetes type 2. There are various classes of oral medications available that help lower blood sugar levels by different mechanisms. These medications include:
- Metformin: This commonly prescribed medication improves insulin sensitivity and reduces glucose production in the liver.
- Sulfonylureas: These medications stimulate the pancreas to produce more insulin.
- DPP-4 inhibitors: These drugs enhance insulin release and reduce glucose production.
- GLP-1 receptor agonists: Injected or oral medications that stimulate insulin release, suppress glucagon secretion, and slow gastric emptying.
- SGLT2 inhibitors: These medications help the kidneys excrete excess glucose through urine.
In certain cases, insulin therapy may be required to manage blood sugar effectively. Insulin can be administered via injections or insulin pumps, and the dosage and timing are customized for individual needs.
Diet and Nutrition
A healthy diet is vital in the treatment and management of diabetes type 2. Focus on consuming nutrient-rich foods while limiting the intake of processed and sugary foods. Consider the following dietary recommendations:
- Choose complex carbohydrates like whole grains, legumes, and vegetables over refined carbohydrates.
- Include lean proteins such as fish, poultry, and tofu in your meals.
- Opt for healthy fats like avocados, nuts, and olive oil.
- Avoid sugary beverages and stick to water or unsweetened drinks.
- Control portion sizes to maintain a healthy weight and manage blood sugar levels.
It is essential to work with a registered dietitian to create an individualized meal plan that meets your specific dietary needs and helps control blood sugar levels effectively.
Exercise and Physical Activity
Regular exercise is beneficial for managing diabetes type 2 as it helps improve insulin sensitivity and aids in weight management. Consider the following recommendations for incorporating physical activity into your routine:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking or cycling.
- Incorporate strength training exercises two to three times a week to build muscle mass.
- Engage in flexibility and balance exercises, such as yoga or tai chi, to improve overall fitness.
Consult with a healthcare professional before starting an exercise program to ensure it is safe and suitable for your condition and fitness level. Monitoring blood sugar levels before, during, and after exercise is crucial to avoid fluctuations and maintain stable levels.
Achieving Diabetes Remission - How to Cure Diabetes Type 2 Permanently: Complete Guide
Achieving diabetes remission refers to the significant improvement or complete reversal of diabetes symptoms and indicators. It involves adopting various strategies that focus on managing blood sugar levels, promoting weight loss, and making long-term lifestyle changes.
What is Diabetes Remission?
Diabetes remission is a term used to describe a state where blood sugar levels remain within a healthy range without relying on diabetes medication or insulin injections. It signifies a significant improvement in overall health and a reduced risk of diabetes-related complications.
Bariatric Surgery and Weight Loss
Bariatric surgery, also known as weight loss surgery, is a surgical procedure that aids in weight reduction for individuals with severe obesity. It can be a viable option for achieving diabetes remission in certain cases. This procedure helps to control blood sugar levels and improves insulin sensitivity, leading to a higher likelihood of diabetes reversal.
Weight loss, whether achieved through surgery or other methods, plays a crucial role in achieving diabetes remission. Shedding excess pounds helps to decrease insulin resistance, enhance glucose utilization, and restore normal pancreatic function, resulting in improved blood sugar management.
Lifestyle Changes for Diabetes Remission
Adopting healthy lifestyle habits can greatly contribute to achieving diabetes remission. Some key lifestyle changes include:
- Following a balanced and nutritious diet: Consuming a variety of whole foods, controlling portion sizes, and limiting refined sugars and carbohydrates.
- Incorporating regular physical activity: Engaging in aerobic exercises, strength training, and other physical activities that promote weight loss and improve insulin sensitivity.
- Managing stress levels: Practicing stress-reducing techniques such as meditation, yoga, or engaging in hobbies and activities that bring joy.
- Getting quality sleep: Prioritizing a consistent sleep schedule and aiming for 7-8 hours of restful sleep each night.
- Quitting smoking and limiting alcohol consumption: Smoking adversely affects blood sugar control, while excessive alcohol intake can lead to weight gain and high blood sugar levels.
By incorporating these lifestyle changes, individuals with Type 2 Diabetes can significantly improve their overall health and increase the chances of achieving remission from diabetes.
Managing Diabetes Type 2 - How to Cure Diabetes Type 2 Permanently: Complete Guide
Managing diabetes type 2 requires careful attention to blood sugar control, regular monitoring, and adopting a healthy lifestyle. By effectively managing the condition, individuals can minimize complications and enhance their overall well-being.
Blood Sugar Control
Achieving and maintaining optimal blood sugar levels is crucial for managing diabetes type 2. Here are some key strategies that can help:
- Dietary choices: Focus on consuming a balanced diet that is low in refined sugars and carbohydrates. Include plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats. Portion control and meal planning can assist in regulating blood sugar levels.
- Regular exercise: Engaging in physical activity, such as brisk walking, cycling, or swimming, can improve insulin sensitivity and aid in blood sugar control. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Medication adherence: Take prescribed medications as instructed by healthcare professionals. These may include oral medications or insulin injections to help regulate blood sugar levels.
Monitoring and Self-Care
Regular monitoring and self-care play a vital role in effectively managing diabetes type 2. Consider the following:
- Glucose monitoring: Check blood sugar levels regularly using a glucose meter or continuous glucose monitoring system. This helps track progress and enables adjustments to medication, diet, and activity levels as needed.
- Stress management: Stress can impact blood sugar levels, so finding healthy coping mechanisms such as deep breathing exercises, meditation, or engaging in hobbies can be beneficial.
- Foot care: Pay attention to foot health by practicing good hygiene, wearing comfortable and supportive footwear, and regularly inspecting feet for any signs of injury or infection.
- Regular check-ups: Schedule regular appointments with healthcare professionals to monitor overall health, discuss any concerns, and receive necessary screenings or vaccinations.
Living with Diabetes
Living with diabetes type 2 involves making long-term lifestyle changes and adopting healthy habits. Consider the following tips:
- Education and support: Stay informed about diabetes management through reliable sources and participate in support groups or educational programs to learn from others and share experiences.
- Emotional well-being: Manage stress, seek emotional support when needed, and prioritize self-care activities that promote mental and emotional well-being.
- Social interactions: Maintain an active social life and communicate with loved ones about diabetes to receive the necessary understanding and support.
Remember, effectively managing diabetes type 2 requires a holistic approach that incorporates dietary choices, regular exercise, medication adherence, monitoring, self-care, and adopting a positive mindset. By proactively addressing the condition, individuals can lead fulfilling lives while minimizing the impact of diabetes on their overall health. (Note: This text is a fictional representation and should not be considered as medical advice. Please consult a healthcare professional for personalized guidance and treatment.)
Diabetes Type 2 Resources and Support - How to Cure Diabetes Type 2 Permanently: Complete Guide
When dealing with Type 2 Diabetes, having access to reliable resources and support is essential for effectively managing the condition. Below, you will find valuable information and links to trusted sources that can help you navigate your diabetes journey:
Diabetes UK: A Valuable Resource
Diabetes UK is a renowned organization dedicated to supporting individuals with diabetes. Their website provides a wealth of resources, including educational materials, practical guides, and the latest research updates. You can find valuable information on managing diabetes, healthy eating, exercise tips, and much more.
Useful Information and Links
Below are some additional trusted sources and links that can provide essential information and support:
- American Diabetes Association (ADA): ADA offers comprehensive resources, including educational materials, support groups, and tips for managing diabetes. Visit their website for tools on nutrition, exercise, and self-care.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): NIDDK provides reliable information on diabetes-related research, clinical trials, and treatment options. Explore their website for insights into diabetes management, prevention, and potential breakthroughs.
- Mayo Clinic: The Mayo Clinic website features in-depth articles, expert advice, and practical tips on various aspects of diabetes management. Discover their resources on diabetes care, complications, and prevention strategies.
Getting in Touch and Seeking Help
When facing challenges or needing support, you can reach out to healthcare professionals and support groups specializing in diabetes care. Here are steps to take:
- Contact your primary care physician or endocrinologist for personalized guidance and medical advice tailored to your specific needs.
- Seek out local support groups or organizations that offer community and emotional support for individuals with diabetes. Connecting with others who understand your journey can greatly enhance your well-being.
- If you're struggling emotionally or mentally with diabetes management, consider reaching out to a mental health professional who can provide guidance and support.
Remember that managing diabetes effectively requires a multidimensional approach, and it's okay to seek help and leverage available resources. Take advantage of these valuable resources and support systems to empower yourself and live a fulfilling life with Type 2 Diabetes.