
Stem Cells and Diabetes






Islet Cell Transplantation
Research and Future Advancements for Diabetes: How to Cure Diabetes in the US
Diabetes research is constantly evolving, with promising advancements on the horizon. This article provides an overview of the current understanding of diabetes, existing treatments, and the role of GLP-1 in diabetes management. Additionally, it explores future advancements in gene therapy, stem cell therapy, and nanotechnology. Lifestyle interventions and prevention strategies are also discussed, highlighting the importance of exercise, dietary recommendations, and education. The challenges and opportunities in diabetes research are highlighted, with a focus on funding, collaboration, and ethical considerations. Explore the latest in diabetes research and future possibilities.
Understanding Diabetes
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels. In this section, we will delve into different aspects of diabetes to gain a better understanding of the disease.
Types of Diabetes
There are several types of diabetes, with the most common ones being type 1 diabetes, type 2 diabetes, and gestational diabetes.
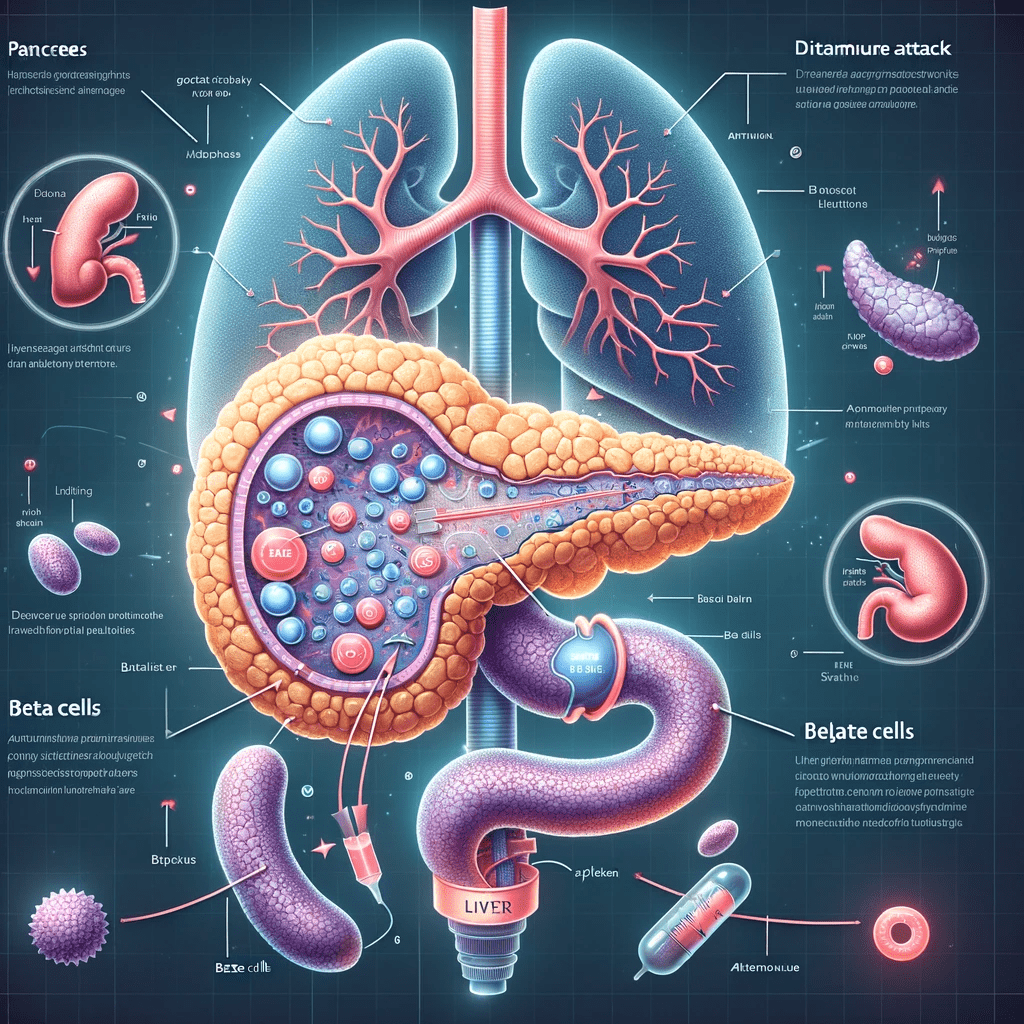
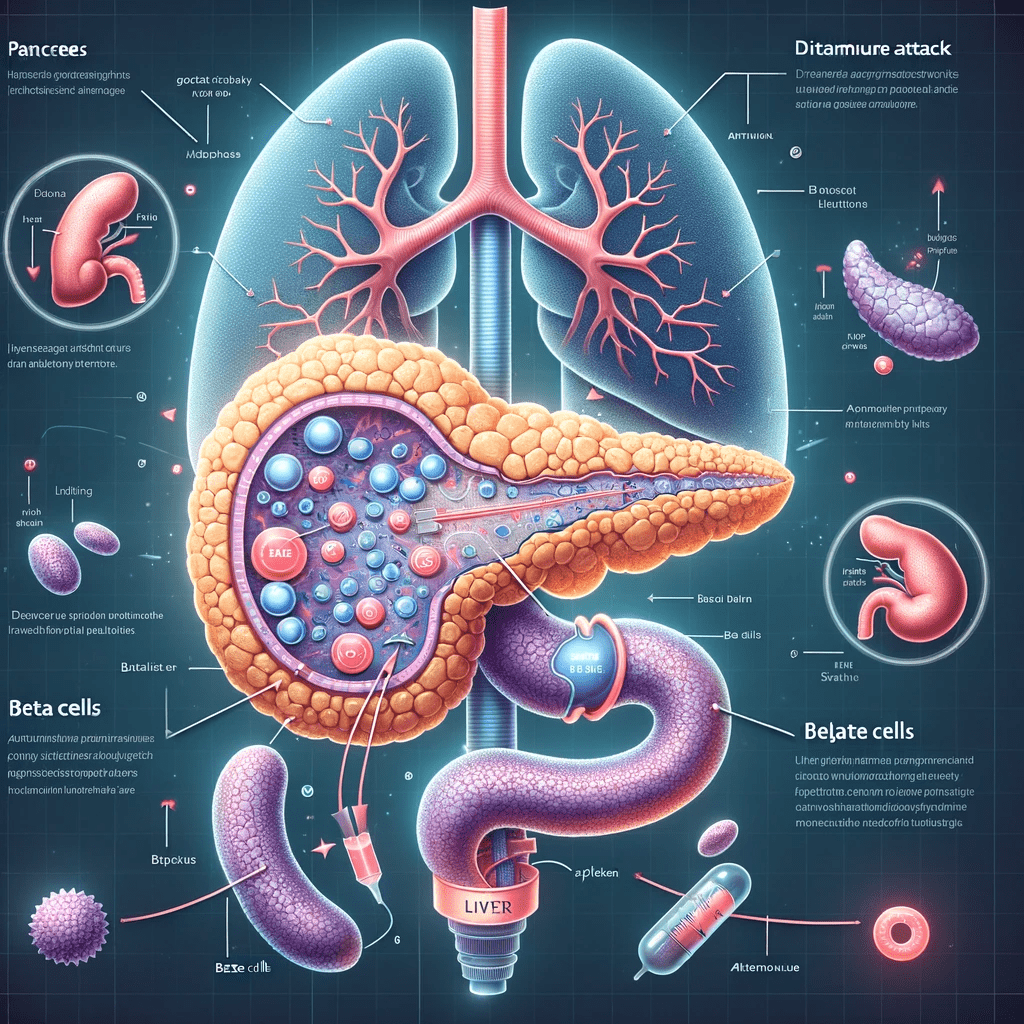
- Type 1 diabetes: This form of diabetes occurs when the body's immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. As a result, the pancreas produces little to no insulin, leading to elevated blood sugar levels.
- Type 2 diabetes: Type 2 diabetes occurs when the body becomes resistant to the effects of insulin or when the pancreas fails to produce enough insulin to meet the body's needs. This is often associated with lifestyle factors such as poor diet, sedentary lifestyle, and obesity.
- Gestational diabetes: Gestational diabetes develops during pregnancy and usually resolves after childbirth. However, women who have had gestational diabetes are at increased risk of developing type 2 diabetes in the future.
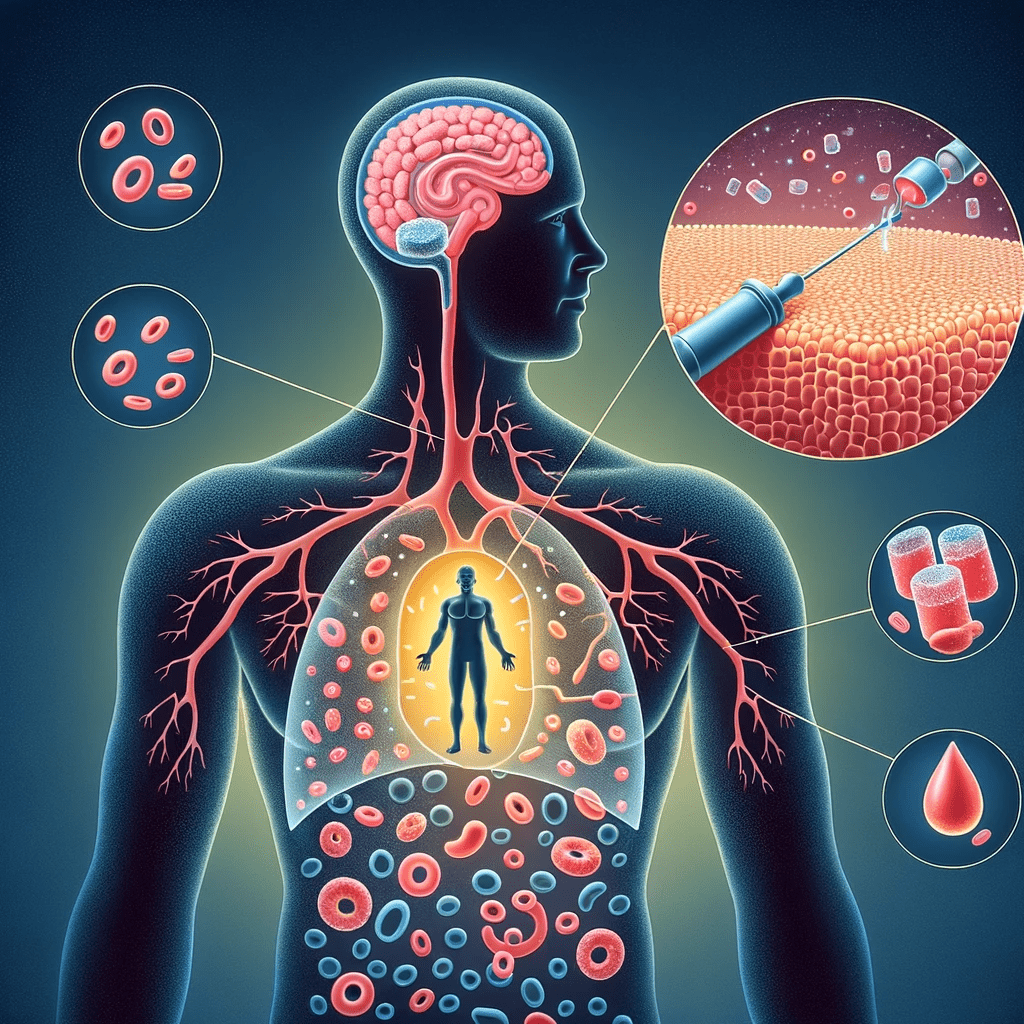
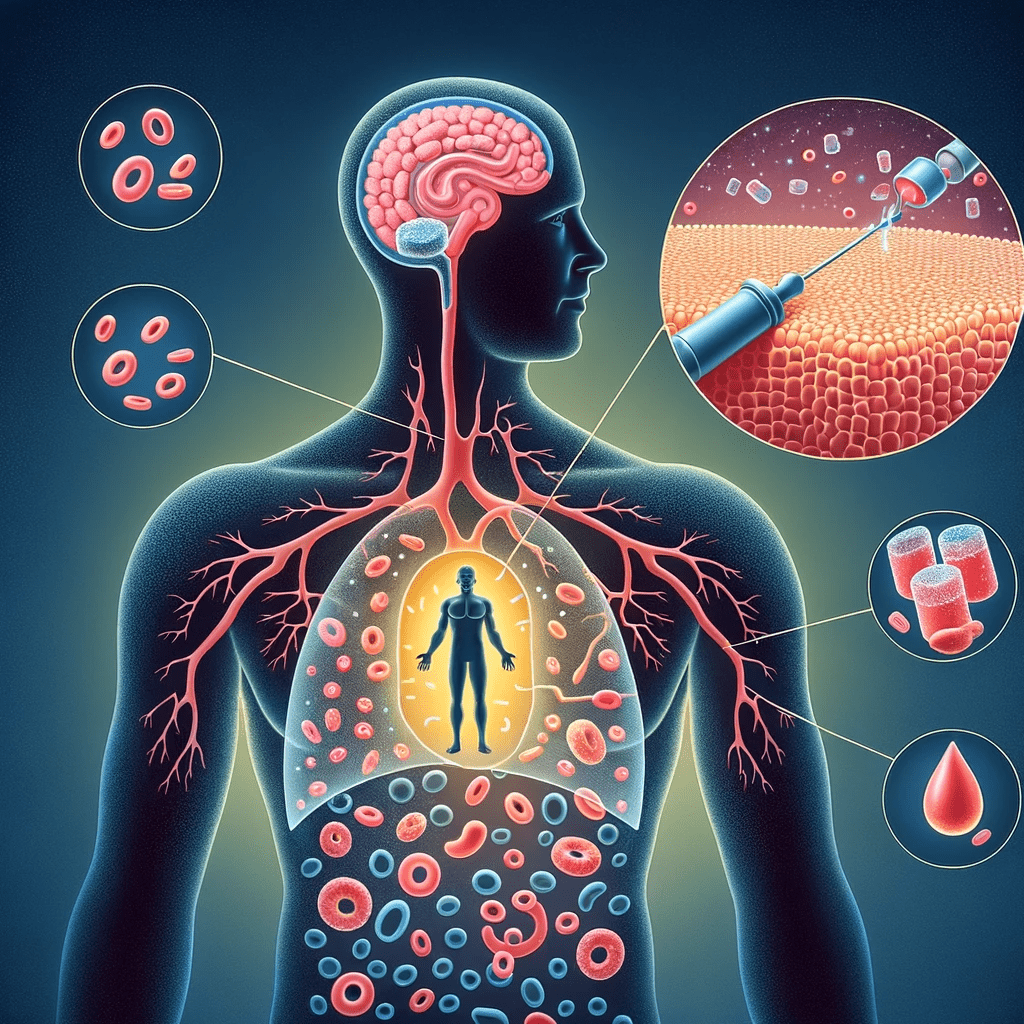
Mechanisms of Insulin and Glucagon Regulation
Insulin and glucagon are hormones that play a crucial role in regulating blood sugar levels.
- Insulin: Insulin is produced and released by the beta cells of the pancreas. Its primary function is to facilitate the uptake of glucose from the bloodstream into cells, where it can be used as a source of energy. Insulin also helps to store excess glucose in the liver and muscles for later use.
- Glucagon: Glucagon, on the other hand, is produced and released by the alpha cells of the pancreas. Its main role is to raise blood sugar levels by stimulating the liver to convert stored glycogen into glucose and release it into the bloodstream.
Glucose Metabolism and its Role in Diabetes
Glucose metabolism is the process by which the body breaks down and utilizes glucose for energy. In individuals without diabetes, this process is tightly regulated to maintain blood sugar levels within a normal range.
- After a meal, carbohydrates are broken down into glucose, which is then absorbed into the bloodstream.
- Insulin is released in response to the rise in blood glucose levels, allowing the glucose to enter cells and be used as energy.
- In individuals with diabetes, there is a disruption in glucose metabolism. In type 1 diabetes, insulin production is impaired, leading to inadequate uptake of glucose by cells. In type 2 diabetes, insulin resistance and/or inadequate insulin production hinder glucose uptake.
- This results in elevated blood sugar levels, which, if not properly managed, can lead to various complications over time.
Understanding the different types of diabetes and the mechanisms behind insulin and glucagon regulation is crucial in developing effective treatment strategies and interventions for individuals living with diabetes.
Current Treatments for Diabetes
In managing diabetes, various treatment options are available to help individuals maintain stable blood sugar levels and improve overall health. This section explores different approaches, including insulin therapy, oral medications, lifestyle modifications, and highlights the challenges and limitations associated with existing treatments.
Insulin Therapy and Glucose Monitoring
Insulin therapy remains a cornerstone in diabetes management, especially for individuals with type 1 diabetes or advanced type 2 diabetes. Injected subcutaneously or delivered through insulin pumps, insulin helps regulate blood sugar levels by facilitating the uptake of glucose into cells. Monitoring blood glucose levels frequently is crucial to determine the appropriate insulin dosage and ensure optimal glycemic control.
Oral Medications for Diabetes
In addition to insulin therapy, oral medications are available for individuals with type 2 diabetes to improve blood sugar control. These medications work through various mechanisms, such as stimulating insulin production, reducing glucose production in the liver, and increasing insulin sensitivity in cells. Metformin, sulfonylureas, DPP-4 inhibitors, and SGLT-2 inhibitors are commonly prescribed oral medications.
Lifestyle Modifications and Dietary Approaches
Alongside medication and insulin therapy, lifestyle modifications play a crucial role in diabetes management. Regular physical activity, such as aerobic exercises and strength training, helps improve insulin sensitivity and control weight. A balanced and nutritious diet, emphasizing whole grains, lean proteins, fruits, and vegetables, can help regulate blood sugar levels and support overall health. Additionally, portion control, carbohydrate counting, and mindful eating techniques can aid in managing blood glucose levels effectively.
Challenges and Limitations of Existing Treatments
While current treatments for diabetes provide valuable tools for managing the condition, they also pose challenges and limitations. Insulin therapy can be complex, requiring careful dose adjustments and potentially causing hypoglycemia if not managed properly. Oral medications may have side effects and may not be suitable for individuals with certain medical conditions. Additionally, lifestyle modifications may be challenging to adopt and sustain long-term.
- Insulin therapy remains a cornerstone in diabetes management, especially for individuals with type 1 or advanced type 2 diabetes.
- Oral medications can help improve blood sugar control for individuals with type 2 diabetes.
- Lifestyle modifications, including regular exercise and a balanced diet, are essential in managing diabetes.
- Existing treatments have challenges and limitations that need to be addressed for optimal diabetes management.
The Role of GLP-1 in Diabetes
GLP-1, short for glucagon-like peptide-1, plays a crucial role in diabetes management. This peptide hormone is produced by specific cells in the intestine and the brain, and it exerts various regulatory and protective effects on glucose metabolism.
Introduction to GLP-1 and its Functions
GLP-1 is derived from the tissue-dependent post-translational processing of proglucagon peptide. The initial product, GLP-1(1-37), undergoes amidation and proteolytic cleavage, resulting in two biologically active forms: GLP-1(7-36) amide and GLP-1(7-37). With a protein-like secondary structure, GLP-1 consists of two α-helices separated by a linker region.
The expression of the proglucagon gene, which encodes GLP-1, can be found in several organs including the pancreas, intestine, and brain. Pancreatic proglucagon gene expression is promoted during fasting and hypoglycemia, while intestinal proglucagon gene expression is reduced during fasting and stimulated by food intake.
GLP-1 Receptor Agonists in Diabetes Treatment
To enhance the activity of GLP-1, researchers have developed GLP-1 receptor agonists as pharmaceutical agents for diabetes treatment. These agonists bind to and activate the GLP-1 receptors in various tissues, leading to increased insulin secretion, reduced gastric emptying, and improved postprandial glycemic control. The use of GLP-1 receptor agonists has shown potential benefits, including weight loss and a lower risk of hypoglycemia, compared to other treatment options.
Clinical Trials and Efficacy of GLP-1-Based Therapies
Clinical trials have evaluated the efficacy and safety of GLP-1-based therapies in the treatment of diabetes. These trials have demonstrated significant improvements in glycemic control, reduction in HbA1c levels, and enhanced β-cell function. GLP-1-based therapies have also been associated with cardiovascular benefits, such as reduced risk of major adverse cardiovascular events.
It is essential to note that GLP-1 has a short half-life of approximately 2 minutes, as it undergoes rapid degradation by enzymes such as dipeptidyl peptidase-4 (DPP-4) and neutral endopeptidase 24.11 (NEP 24.11). However, even with its short half-life, GLP-1 retains enough activity to activate its receptors and exert its beneficial effects.
Future Advancements in Diabetes Research
The field of diabetes research is constantly evolving, with ongoing efforts to develop innovative approaches to improve treatment and management. Several promising advancements on the horizon show potential in revolutionizing the way we understand and address diabetes. This section explores some of these exciting future prospects, including gene therapy, stem cell therapy, artificial pancreas and closed-loop systems, and nanotechnology in diabetes treatment.
Gene Therapy and Genetic Approaches
Gene therapy holds immense promise in the treatment of diabetes. By directly targeting the genetic factors underlying the disease, researchers aim to develop therapies that can correct or modify genes associated with impaired insulin production or function. Through precise gene editing techniques, such as CRISPR-Cas9, scientists have the potential to permanently address the root causes of diabetes, offering long-term solutions for patients.
Stem Cell Therapy for Diabetes
Stem cell therapy offers a regenerative approach to treating diabetes by replenishing the body's insulin-producing cells. Researchers are exploring various sources of stem cells, including embryonic stem cells, induced pluripotent stem cells, and adult stem cells, to generate functional pancreatic beta cells. By transplanting these cells into individuals with diabetes, it is hoped that they can restore insulin production and regulate blood sugar levels, providing a potential cure for the disease.
Artificial Pancreas and Closed-Loop Systems
The development of artificial pancreas systems aims to mimic the physiological function of a healthy pancreas in people with diabetes. These systems combine continuous glucose monitoring (CGM) devices with insulin pumps, using sophisticated algorithms to automatically adjust insulin delivery based on real-time glucose readings. Closed-loop systems provide a more automated and precise approach to insulin administration, offering improved blood sugar control and reducing the burden of diabetes management.
Nanotechnology in Diabetes Treatment
Nanotechnology holds significant potential in revolutionizing diabetes treatment. By utilizing tiny particles and devices at the nanoscale, researchers can enhance drug delivery systems, develop novel glucose sensing technologies, and improve the efficiency of insulin administration. Nanomedicine approaches, such as smart insulin patches and glucose-responsive nanoparticles, offer new avenues for personalized and targeted diabetes therapies, maximizing effectiveness while minimizing side effects.
Lifestyle Interventions and Prevention Strategies
The section on lifestyle interventions and prevention strategies explores various approaches to manage and prevent diabetes through exercise, diet, education, and behavioral interventions.
Exercise and Physical Activity
Regular physical activity plays a crucial role in managing diabetes and reducing the risk of developing the condition. Engaging in exercises such as brisk walking, cycling, swimming, or strength training can help improve insulin sensitivity, regulate blood sugar levels, and promote weight loss or maintenance.
Incorporating at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, spread across several days, is recommended for individuals with diabetes. Additionally, strength training exercises that target major muscle groups should be performed at least twice a week.
Dietary Recommendations for Diabetes Prevention
A healthy diet is essential in the prevention and management of diabetes. Emphasizing a balanced eating pattern with a focus on whole foods, fiber-rich carbohydrates, lean proteins, and healthy fats can help regulate blood sugar levels and promote overall well-being.
Key dietary recommendations include limiting the intake of sugary beverages, refined grains, processed foods, and saturated fats. Instead, individuals should opt for a variety of fruits, vegetables, whole grains, legumes, lean meats, and low-fat dairy products. Portion control and mindful eating practices are also essential for managing caloric intake and preventing excessive weight gain.
Education and Behavioral Interventions
Education and behavioral interventions play a vital role in empowering individuals to make informed decisions about their health and adopt healthy lifestyle habits.
Diabetes education programs provide individuals with comprehensive information about diabetes management, including medication adherence, blood sugar monitoring, healthy eating, and stress management. These programs also address the emotional and psychological aspects of living with diabetes and provide support networks for individuals and their families.
Additionally, behavioral interventions focus on goal setting, problem-solving, and motivation to promote sustainable behavior change. Techniques such as cognitive-behavioral therapy, motivational interviewing, and self-monitoring help individuals overcome barriers and develop effective coping strategies for managing diabetes.
Challenges and Opportunities in Diabetes Research
Funding and Support for Diabetes Research
Funding for diabetes research plays a crucial role in advancing our understanding of the disease and developing innovative treatments. Securing adequate funding is a prominent challenge in the field, as research projects require significant financial resources to conduct rigorous studies and trials.
In recent years, there has been a growing recognition of the importance of diabetes research, leading to increased funding opportunities from governmental organizations, private foundations, and pharmaceutical companies. However, the competition for funding remains fierce, and researchers must demonstrate the potential impact and feasibility of their projects to secure financial support.
Collaborative efforts between research institutions, industry partners, and advocacy groups are also essential for driving advancements in diabetes research. By pooling resources and expertise, collaborative initiatives can tackle complex research questions and accelerate the development of new therapies and preventive strategies.
Collaboration and Data Sharing in the Field
Collaboration and data sharing are vital components of diabetes research, fostering a collective approach to tackle the challenges associated with the disease. Collaborative networks allow researchers to share knowledge, resources, and data, facilitating the generation of robust evidence and enabling the replication of findings across different populations.
Data sharing initiatives contribute to the development of comprehensive databases that encompass various aspects of diabetes, including genetic information, clinical data, and treatment outcomes. Access to rich, diverse datasets can uncover new insights, identify risk factors, and improve personalized treatment approaches.
However, challenges persist in terms of data sharing frameworks, privacy concerns, and intellectual property rights. Establishing standardized protocols and ethical guidelines is crucial to ensure responsible data sharing while safeguarding the privacy and confidentiality of individuals participating in research studies.
Ethical Considerations in Diabetes Research
As the field of diabetes research advances, ethical considerations become increasingly important to protect the rights and well-being of participants and the integrity of the scientific process. Researchers must adhere to strict ethical standards and obtain informed consent from individuals involved in clinical trials and data collection.
Ensuring inclusivity and diversity in research studies is another important ethical consideration. Diabetes disproportionately affects certain populations, and research efforts should actively include individuals from diverse backgrounds to ensure that interventions and treatments are universally effective.
Transparency and adherence to research ethics boards' guidelines are essential throughout the research process. Responsible conduct in diabetes research helps maintain public trust, ensures participant safety, and allows the dissemination of reliable and trustworthy findings.Overall, navigating the challenges and seizing opportunities in diabetes research requires a collaborative, well-funded, and ethically-driven approach. By addressing these challenges, researchers can pave the way for future advancements in understanding and treating diabetes.
