Diabetes is not only a physical health challenge but also a condition that can take a significant mental and emotional toll on those affected. Living with diabetes requires daily attention to medication, diet, and exercise, which can be overwhelming and lead to feelings of anxiety and depression. Understanding the mental impact of this condition is crucial for comprehensive care and improved quality of life.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- Understanding the Mental Impact of Diabetes
- How Does Diabetes Affect Your Mental Health?
- Common Mental Health Issues in Diabetes Patients
- The Links Between Diabetes and Depression
- Anxiety Disorders and Diabetes
- Coping with Diabetes-Related Stress
- Managing Diabetes and Mental Health Simultaneously
- Involving Family in Diabetes Care
- Exploring Related Concerns on Diabetes and Mental Health
Understanding the Mental Impact of Diabetes
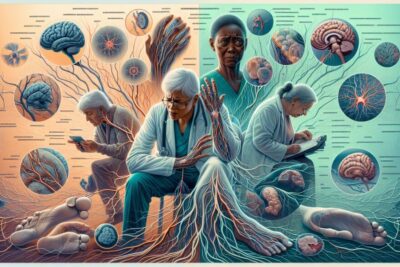
Living with diabetes goes beyond just managing blood sugar levels; it encompasses dealing with emotional and psychological challenges that arise from the condition. The constant monitoring, treatment decisions, and potential complications can lead to a significant mental burden, affecting a person's mood, relationships, and overall psychological well-being.
The need to cope with chronic illness management daily can lead to feelings of burnout, frustration, and isolation. Recognizing and addressing these psychological needs is essential for those living with diabetes to improve not only their medical outcomes but their mental health as well.
Support systems and proper management strategies are imperative to help individuals navigate the complexities of this chronic condition.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!










How Does Diabetes Affect Your Mental Health?
Diabetes can lead to a variety of mental health challenges, including depression, anxiety, and eating disorders. Fluctuations in blood glucose levels can directly impact mood and cognitive function, sometimes resulting in irritability or a sense of lethargy. The fear of hypoglycemic episodes can contribute to ongoing anxiety, while the demands of managing the disease can trigger depressive symptoms.
Additionally, the stress of persistent medical care can exacerbate existing mental health issues or even lead to the development of new ones. It is critical to recognize these potential impacts early on to provide timely and appropriate interventions.
Studies have shown that individuals with diabetes have a higher prevalence of depression compared to the general population. This underlines the importance of mental health screenings as part of routine diabetes care.
Common Mental Health Issues in Diabetes Patients
- Depression
- Anxiety disorders
- Eating disorders, such as binge eating or bulimia
- Diabetes distress, a term used to describe the unique emotional burden of managing diabetes
- Cognitive impairment in cases of severe or uncontrolled diabetes
The Links Between Diabetes and Depression
There is a well-documented connection between diabetes and depression. Depression can negatively affect diabetes management, leading to poorer health outcomes and reduced quality of life. The presence of depression in diabetes patients can result in reduced adherence to treatment plans, leading to higher A1C levels and increased risk for diabetes-related complications.
Understanding the bidirectional relationship between diabetes and depression is crucial for healthcare providers. This knowledge allows for the development of treatment plans that address both conditions simultaneously, potentially improving both mental health and glycemic control.
Encouraging self-management and fostering a sense of empowerment can be effective in reducing the incidence of depression in individuals with diabetes.
Anxiety Disorders and Diabetes
Anxiety can manifest in many forms for those with diabetes, from generalized anxiety disorder to panic attacks or specific phobias related to diabetes care, such as needle phobia. The chronic nature of diabetes can lead to constant worry about the future and fear of complications, which may trigger or worsen anxiety symptoms.
Effective management of anxiety in diabetic patients includes cognitive-behavioral therapy, medication, and relaxation techniques, as well as diabetes education to reduce fears related to the disease.
Peer support groups can also be beneficial, providing a space for individuals to share experiences and coping strategies.
Stress management is an essential component of diabetes care. Chronic stress can affect blood glucose levels, making it harder to manage diabetes effectively. It is important for individuals to identify stressors and develop healthy coping mechanisms.
Techniques such as mindfulness, exercise, and hobbies can provide outlets for stress relief. Additionally, diabetes self-management education and support (DSMES) programs can equip patients with the knowledge and skills needed to reduce stress associated with disease management.
Professional counseling might be necessary for some individuals to help them cope with the intricate challenges of living with diabetes.
Managing Diabetes and Mental Health Simultaneously
Effective diabetes management includes addressing both physical and mental health. A holistic approach involves regular screening for mental health issues, integrated care strategies, and patient education to ensure that mental health is not neglected.
Collaborative care models that include a team of healthcare providers, such as endocrinologists, primary care physicians, mental health professionals, diabetes educators, and dietitians, can offer comprehensive support.
Lifestyle interventions, such as exercise and dietary changes, can also have positive effects on both blood sugar control and mental health.
Involving Family in Diabetes Care
Family involvement in diabetes management can provide vital support and improve health outcomes. Education and open communication are key to helping family members understand the complexities of diabetes care and how they can assist.
Family therapy and family-based interventions can be useful in addressing interpersonal issues that may arise and enhancing family support systems.
Moreover, involving family members in medical appointments and educational sessions can lead to better understanding and more cohesive care, reducing the mental toll on the individual with diabetes.
As we delve deeper into the subject of diabetes and its impacts on mental health, watch this insightful video that shares personal experiences and professional insights:
How Does Diabetes Affect You Mentally?
Diabetes affects individuals mentally through the constant demands of management, fear of complications, and its potential to exacerbate or trigger mental health conditions. The psychological toll of living with diabetes includes a higher risk for depression, anxiety, and eating disorders.
The influence of blood glucose fluctuations on cognitive function can also lead to difficulties in concentration, decision-making, and can cause mood swings, further impacting mental health.
What Should Diabetics Drink First Thing in the Morning?
Diabetics should opt for non-sugary, low-calorie drinks like water or herbal tea first thing in the morning. These beverages can help to maintain hydration without affecting blood sugar levels. It is also essential for diabetics to avoid high-carbohydrate or sugary drinks that could cause blood sugar spikes.
A glass of water with a squeeze of lemon can be refreshing and may help with glucose control. Consultation with a healthcare provider can offer personalized advice.
How Does Diabetes Affect the Mind?
Diabetes can affect the mind through neurological changes caused by fluctuating glucose levels, potentially leading to cognitive impairment. Chronic hyperglycemia can harm brain function, contributing to decreased mental flexibility, slower mental speed, and challenges with memory.
Furthermore, the psychological burden and stress of managing diabetes can lead to mental fatigue, impacting overall cognitive function.
What Are the Psychological Burdens of Diabetes?
The psychological burdens of diabetes include the constant need for vigilance in managing the disease, the fear of complications, and the impact on social and personal relationships. These burdens can manifest as diabetes distress, depression, anxiety, and other mental health issues.
Understanding these burdens is critical for healthcare providers to support their patients holically, helping them to maintain not only physical health but mental well-being too.
By acknowledging The Mental Toll of Diabetes and implementing strategies to mitigate it, individuals living with diabetes and their families can work towards a more balanced and fulfilling life. Health professionals play a crucial role in recognizing the signs of mental health struggles in diabetic patients and providing appropriate care and support.
✨ Other articles you might be interested in:
- Understanding the Differences: Ophthalmologist, Optometrist, Retina Specialist? What's the Difference?
- Understanding serious foot problems and diabetes
- Understanding diabetes and foot problems
- Exploring the Potential: Can Anti-Ageing Drugs Treat Foot Ulcers?
- Understanding and managing steroid-induced diabetes



