Diabetes is a complex condition that affects various aspects of life, including sexual health. It's no secret that managing diabetes can be challenging, but it's important to recognize its potential impact on intimacy and relationships.
While discussions about blood sugar levels and diet are commonplace, conversations regarding sex and diabetes are often neglected. Yet, understanding how diabetes interplays with sexual well-being is crucial for maintaining a fulfilling life.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- How Does Diabetes Affect Sexual Health?
- Tips for Maintaining Intimacy With Diabetes
- Dealing With Erectile Dysfunction and Diabetes
- Understanding the Impact of Diabetes on Libido
- How to Manage Blood Sugar Levels During Sex
- Getting Support: Talking to Healthcare Providers About Sexual Issues
- Understanding Sex and Diabetes | ADA: Addressing Common Questions
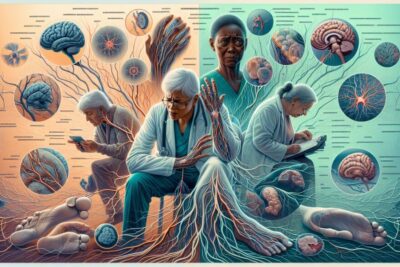
How Does Diabetes Affect Sexual Health?
Diabetes can lead to a range of complications, and sexual health is no exception. High blood glucose levels can damage blood vessels and nerves, which are critical for sexual arousal and response. Additionally, the emotional stress of managing a chronic illness can affect sexual desire and performance.
For men, diabetes is commonly associated with erectile dysfunction, making it difficult to achieve or maintain an erection. Women may experience vaginal dryness or discomfort during sex, which can stem from imbalances in blood sugar. Moreover, fluctuations in blood sugar levels can lead to fatigue, which can dampen sexual enthusiasm.
It's not just the physical side; diabetes can also have psychological effects. Anxiety and depression are more prevalent in individuals with diabetes, and these emotional states can further complicate sexual intimacy.
Despite these challenges, there are ways to manage and mitigate the effects of diabetes on sexual health. The key is to address both the physical and emotional aspects proactively.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!










Tips for Maintaining Intimacy With Diabetes
Maintaining a healthy sexual relationship while managing diabetes involves open communication with your partner. Discussing your concerns and experiences can alleviate stress and build a stronger connection.
Regular exercise and a balanced diet can improve blood glucose control, which in turn, can enhance sexual function. It's also important to consider timing; blood sugar levels can affect energy and arousal, so plan intimate moments accordingly.
Experimenting with different positions and activities can reduce discomfort and increase pleasure. Lubricants and other aids can be helpful for women experiencing vaginal dryness due to diabetes-related hormonal changes.
Lastly, carve out time for intimacy. It's easy for the routine management of diabetes to overshadow personal relationships, but prioritizing time with your partner can strengthen your bond and improve your sexual health.
Dealing With Erectile Dysfunction and Diabetes
Erectile dysfunction (ED) can be a sensitive topic, but it's a common issue for men with diabetes. The first step in dealing with ED is to consult with a healthcare provider to explore the underlying causes and potential treatments.
Medications such as phosphodiesterase type 5 (PDE5) inhibitors are effective for many men. However, it's vital to check with your doctor, especially if you're on heart medications, as there can be interactions.
- Lifestyle changes, like quitting smoking and reducing alcohol consumption, can improve ED.
- Exercise, particularly aerobic activities, can enhance cardiovascular health and therefore, erectile function.
- Pelvic floor exercises have been shown to benefit men suffering from ED.
It's also essential to manage psychological factors. Stress and anxiety can exacerbate ED, so consider counseling or therapy to address these aspects.
Understanding the Impact of Diabetes on Libido
Diabetes can lead to low libido in both men and women. Hormonal imbalances, particularly low testosterone levels in men, can diminish sexual desire. In women, hormonal changes can make sex uncomfortable or less enjoyable, leading to a decreased interest.
Addressing low libido starts with managing your diabetes effectively. Keeping blood sugar levels within target ranges can help maintain hormonal balance. Speaking with a healthcare provider about possible hormone therapy or other treatments can also be beneficial.
Exploring new ways to connect with your partner and reigniting romance can spark desire. Intimacy isn't limited to sex—cuddling, kissing, and other forms of physical touch can enhance closeness and boost libido.
Don't overlook the impact of mental health on libido. Therapy or support groups can provide coping strategies to manage the emotional toll of diabetes.
How to Manage Blood Sugar Levels During Sex
Sexual activity is a form of physical exercise and can affect blood sugar levels. It's important to check blood sugar before and after sex to ensure it remains in a safe range.
Having a snack on hand can help prevent hypoglycemia, especially if you're using insulin or other medications that lower blood sugar. It's also helpful to stay hydrated and take breaks as needed.
Adjusting your diabetes management plan for sexual activity can be discussed with a healthcare provider. They can offer personalized advice on medication timing and glucose monitoring.
Wearing a continuous glucose monitor (CGM) during sex can allow for real-time glucose tracking without interruption. This technology can provide peace of mind and reduce worry about potential glucose fluctuations.
Remember, communication with your partner is key. Let them know how diabetes may affect your sexual activity and what they can do to help should an issue arise.
Getting Support: Talking to Healthcare Providers About Sexual Issues
Discussing sexual health with a healthcare provider can be daunting, but it's a crucial step in managing diabetes-related sexual issues. Be honest about your concerns and symptoms to get the most effective help.
Your provider can refer you to specialists, such as urologists or endocrinologists, who have experience treating sexual dysfunction in the context of diabetes.
Lifestyle changes, medications, and other therapies can be recommended by healthcare professionals to address sexual difficulties. They can also provide resources for emotional support, such as counseling or therapy.
Remember, you're not alone. Many people with diabetes face similar challenges, and support groups can offer camaraderie and advice from those who understand your situation.
Understanding Sex and Diabetes | ADA: Addressing Common Questions
Is Sex Good for Diabetics?
Sexual activity can be beneficial for diabetics as it promotes physical exercise, which is key in managing diabetes. It can improve cardiovascular health and lead to better glucose control.
Moreover, the emotional benefits of a healthy sex life, such as reduced stress and improved mood, can contribute to overall well-being. It's important, however, to monitor blood sugar levels and maintain open communication with your partner regarding your health needs.
How Do I Get My Sex Drive Back With Diabetes?
To reclaim your sex drive, focus on establishing good diabetes control. This can help balance hormones and improve energy levels.
Consider consulting with a healthcare provider about possible treatments for low libido, which might include hormone therapy or counseling. Additionally, developing a deeper emotional connection with your partner can rekindle desire and improve sexual satisfaction.
Do Men With Diabetes Have a Hard Time Ejaculating?
Diabetes can affect ejaculation due to nerve damage and blood flow issues. Some men might experience delayed ejaculation or an inability to ejaculate.
Treatments for this condition include medications, counseling, and lifestyle adjustments. A healthcare professional can provide guidance tailored to the individual's needs.
How Long Can I Live With Type 2 Diabetes?
With proper management and lifestyle choices, individuals with type 2 diabetes can live long, healthy lives. It's essential to adhere to treatment plans, engage in regular physical activity, and maintain a balanced diet.
Regular check-ups and monitoring of blood sugar levels play a significant role in preventing complications and maximizing quality of life.
✨ Other articles you might be interested in:
- Understanding Insulin Resistance: Causes, Symptoms, and Management
- Understanding Diabetes and Skin Complications: Risks and Care Tips
- Navigating Commercial Driving and Diabetes: What You Need to Know
- Understanding Diabetes and Pregnancy | ADA Guidelines
- Exploring the Pathophysiological Impact of Nevro HFX™ High-Frequency (10 kHz) Spinal Cord Stimulation for Painful Diabetic Neuropathy



