
Living with diabetes requires careful attention to your health, and this includes taking care of your feet. Diabetes can lead to serious foot problems that, if not managed properly, can result in severe complications, including amputations. Understanding the symptoms, treatments, and daily care is essential for preventing these issues and maintaining a good quality of life.
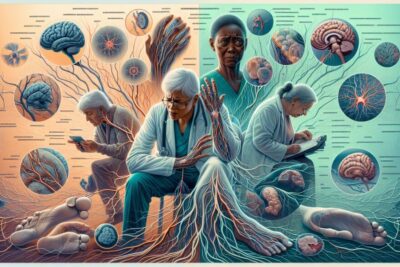
Foot complications are common in diabetic individuals due to the high blood sugar levels that can damage nerves and blood vessels. This can lead to numbness, making it hard to feel injuries, as well as poor circulation, slowing wound healing. Therefore, it's imperative to be proactive about foot health to avoid these serious foot problems and diabetes-related complications.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- How can diabetes affect my feet?
- What are the symptoms of diabetic foot problems?
- How to prevent serious foot problems with diabetes
- When should I see my healthcare provider about foot problems?
- Common treatments for diabetic foot problems
- Tips for daily foot care
- Frequently Asked Questions About Diabetic Foot Problems
How can diabetes affect my feet?
Individuals with diabetes are at risk for nerve damage (neuropathy) and reduced blood flow (peripheral vascular disease), conditions that significantly affect foot health. Neuropathy can cause a loss of sensation, making it difficult to detect injuries or infections. Reduced blood flow can impair the healing process, increasing the chance of ulcers and infections that could lead to amputations if not treated promptly.
Neuropathy also increases the risk of foot deformities like Charcot foot, where bones in the foot weaken and break, leading to changes in foot shape. Additionally, poor circulation can result in gangrene, a serious condition that may require amputation if it spreads. Regular checks and proper foot care are crucial steps in managing diabetic foot conditions.
Keeping blood sugar levels under control is also essential for preventing diabetic peripheral vascular disease, which can lead to painful cramps and tiredness in the legs, hindering everyday activities and further complicating foot health.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!









What are the symptoms of diabetic foot problems?
The symptoms of diabetic foot problems may vary, but common signs include changes in skin color and temperature, pain or cramping in the legs, numbness or tingling, and slow healing sores or cuts. Swelling and redness may also be present, indicating an underlying infection or inflammation.
Skin changes such as dryness, peeling, or cracking, especially around the heels, can be an early warning sign of nerve damage. It is vital to treat these conditions promptly, as even minor skin issues can develop into ulcers or infections if left unchecked.
Discoloration, including redness or darkening of the skin, can point to poor circulation or infection. Severe symptoms, like a deep foot ulcer or the presence of gangrene, constitute a medical emergency and should be addressed by a healthcare provider immediately.
How to prevent serious foot problems with diabetes
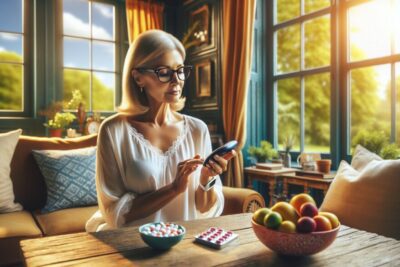
Preventative measures are key in avoiding serious foot problems related to diabetes. Proper foot hygiene and inspection are the first lines of defense. Wash your feet daily, dry them thoroughly, especially between the toes, and apply moisturizer to prevent cracks and dry skin.
Wearing well-fitting shoes is essential. Ill-fitting footwear can cause blisters and sores which can quickly become problematic. It's also important to avoid going barefoot, even at home, to protect your feet from injury.
Managing blood glucose levels is also critical for preventing complications. High blood sugar can damage nerves and blood vessels, leading to the issues discussed earlier. Regular exercise and a well-balanced diet play a significant role in this aspect of diabetic foot care.
When should I see my healthcare provider about foot problems?
If you notice any changes in your feet, it's important to consult with a healthcare provider promptly. Early signs such as cuts that don't heal, persistent pain, or changes in skin color need immediate attention. Any signs of infection like swelling, redness, warmth, or discharge from a wound are also reasons to see a doctor.
For those with diabetes, it's advisable to have regular foot examinations by a professional. During these check-ups, the healthcare provider can identify potential problems early and provide guidance on proper foot care and treatment options.
Common treatments for diabetic foot problems
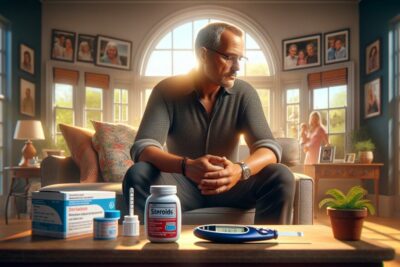
Treatment for diabetic foot problems depends on the severity and type of issue. For minor conditions, such as dry skin or ingrown toenails, regular moisturizing and proper nail care may suffice. More serious problems, like ulcers, may require antibiotics, debridement, and specialized wound care.
In cases of severe neuropathy or poor circulation, a healthcare provider might prescribe medication to manage pain and improve blood flow. Advanced treatments, such as hyperbaric oxygen therapy, may be considered for non-healing wounds.
Tips for daily foot care
Daily foot care is essential for preventing serious complications. Here are some tips:
- Inspect your feet daily for cuts, blisters, redness, or swelling.
- Keep your feet clean and dry, paying special attention to the area between your toes.
- Use a moisturizer to prevent dry skin but avoid applying it between your toes.
- Trim toenails straight across and file the edges to avoid ingrown toenails.
- Wear clean, dry socks and change them daily.
Let's hear from a specialist for more insights on this topic:
Frequently Asked Questions About Diabetic Foot Problems
What are the 5 stages of diabetic foot?
The five stages of diabetic foot include:
- Stage 1: Skin changes and neuropathy without ulceration.
- Stage 2: Formation of ulcers due to minor trauma or pressure.
- Stage 3: Development of deep tissue infection from ulceration.
- Stage 4: Gangrene confined to the local area of the initial ulcer.
- Stage 5: Extensive gangrenous infection requiring potential amputation.
What is diabetic foot syndrome?
Diabetic foot syndrome is a term used to describe the various complications that affect the feet due to diabetes. This can include neuropathy, ulcers, infections, and structural changes like Charcot foot. Managing diabetes effectively and practicing good foot care can help prevent this syndrome.
What do feet look like with diabetes?
Feet affected by diabetes may exhibit a range of symptoms, from dry, cracked skin to more serious conditions such as ulcers or infections. They may also appear reddened or darker due to poor circulation, and in severe cases can develop deformities.
What kind of foot pain does diabetes cause?
Diabetes can cause various types of foot pain, including a dull ache, sharp pain, or burning sensation, primarily due to peripheral neuropathy. It's important to not ignore any persistent foot pain as it may indicate serious underlying issues.
✨ Other articles you might be interested in:



