
Living with diabetes requires constant vigilance to maintain a healthy balance, and unexpected symptoms like dizziness can be both confusing and alarming. For individuals navigating this chronic condition, understanding the connection between dizziness and diabetes is essential for effective management.
From the Diabetes Forum discussions to the latest medical research, the experiences of those with diabetes highlight the multifaceted nature of this symptom. Let's explore what we know about dizziness in the context of diabetes and how to address it.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- Feeling Dizziness in Diabetes: Understanding the Connection
- What Causes Dizziness in Diabetic Patients?
- What to Do If a Diabetic Feels Dizzy?
- Can Diabetes Make You Feel Off Balance?
- How Does Blood Sugar Affect Dizziness?
- What Are the Symptoms of Diabetes-Related Dizziness?
- Can High Blood Sugar Cause Vertigo?
- Frequently Asked Questions About Diabetes and Dizziness
Feeling Dizziness in Diabetes: Understanding the Connection
Those with diabetes may experience dizziness as a symptom of various underlying issues. Dizziness can be an early warning sign of hypoglycemia, a condition characterized by abnormally low blood sugar levels. It's a common misconception that only those on insulin or oral medications can have hypoglycemia; in reality, it can affect anyone with diabetes.
A crucial aspect of managing diabetes is recognizing and understanding symptoms like dizziness. When blood sugar levels plummet, the body reacts by initiating a cascade of physiological responses that can lead to feelings of lightheadedness or vertigo. This is the body’s way of signaling the need to consume glucose.
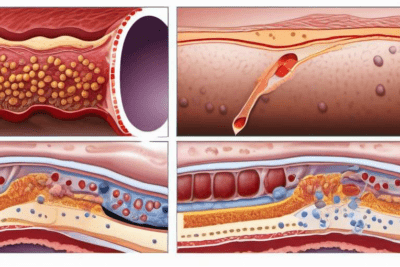
It's not just low blood sugar that can cause problems; high blood sugar levels, or hyperglycemia, can also result in dizziness. When the body is unable to use glucose effectively due to insulin resistance or deficiency, it can lead to dehydration and dizziness.
Furthermore, other factors such as medication side effects, dehydration, or diabetic complications like neuropathy can contribute to feelings of dizziness. It's worth noting that the management of blood sugar levels is a delicate balance, and fluctuations can have a noticeable impact on how a person feels.
Understanding your body's signals and knowing how to respond to them is key to managing diabetes effectively. Frequent monitoring of blood glucose levels can help anticipate and prevent episodes of dizziness before they occur.




Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!
What Causes Dizziness in Diabetic Patients?
The causes of dizziness in diabetic patients are varied and can range from hypoglycemia to other diabetes-related health issues. Skipping meals or not eating enough can precipitate a drop in blood sugar, leading to dizziness. Additionally, intense physical activity without proper adjustments to food intake or medication can cause similar issues.
For those with diabetes, it's not uncommon to experience dizziness as a result of medication side effects. Some diabetes medications can cause blood sugar levels to drop too low, especially if not balanced with food intake.
Low blood pressure, a condition that can be associated with diabetes, is another potential cause of dizziness. This can occur when standing up quickly, known as orthostatic hypotension, leading to a temporary decrease in blood flow to the brain.
Beyond these common triggers, nutritional deficiencies like low levels of important vitamins and minerals can also play a role in feeling dizzy. It's important to maintain a balanced diet rich in all the necessary nutrients to help mitigate these risks.
Addressing these underlying causes is crucial, as persistent dizziness can reduce quality of life and increase the risk of falls and injuries, particularly in older adults.
What to Do If a Diabetic Feels Dizzy?
If you're feeling dizzy and suspect it may be related to your diabetes, the first step is to check your blood sugar levels. If they're low, consuming a quick source of glucose, like juice or glucose tablets, can help alleviate symptoms.
Should hypoglycemia not be the issue, resting for a moment and drinking some water can sometimes help. Dizziness can be a sign of dehydration, which can occur with elevated blood sugar levels.
It is also advisable to sit or lie down to prevent falls and to give your body a chance to recover. Deep, steady breathing may also alleviate the feeling of dizziness by increasing oxygen flow to the brain.
If you experience dizziness frequently, it's important to discuss it with your healthcare provider. They can help determine if your diabetes management plan needs adjusting or if something else might be the cause.
Moreover, don't forget to wear a medical ID bracelet or carry identification that informs others about your diabetes. This can be crucial in an emergency situation if you're unable to communicate.
Can Diabetes Make You Feel Off Balance?
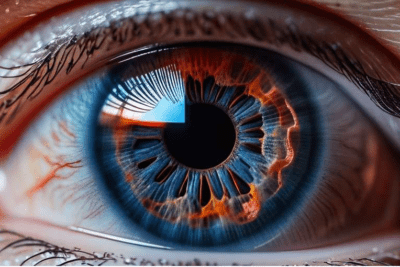
Diabetes can indeed affect your sense of balance, with dizziness being just one manifestation of this. Fluctuating blood sugar levels can impact the inner ear, which plays a key role in maintaining balance.
In addition to blood sugar-related issues, diabetic neuropathy, which is damage to the nerves caused by diabetes, can also impact balance. This condition can lead to weakness, numbness, and pain in the extremities, complicating the body’s ability to maintain equilibrium.
Regular exercise, particularly balance and strength training, can help improve stability and reduce the risk of falls. It's also crucial to manage blood sugar levels effectively to prevent complications that could affect balance.
The use of assistive devices like canes or walkers, as prescribed by a healthcare provider, can help provide stability if balance is significantly impacted. It's essential to create a safe environment by removing tripping hazards and ensuring good lighting at home.
How Does Blood Sugar Affect Dizziness?
The role of blood sugar in dizziness is significant. Both high and low blood sugar levels can cause symptoms that affect equilibrium. Low blood sugar, or hypoglycemia, can lead to symptoms such as dizziness, shaking, and sweating, as the body attempts to signal the need for more glucose.
On the other hand, high blood sugar, or hyperglycemia, can lead to dehydration, as the body tries to rid itself of excess glucose through urine. This dehydration can then result in dizziness and fatigue.
Maintaining consistent blood sugar levels is crucial in preventing these symptoms. Regular monitoring, along with a balanced diet and appropriate medication, can help keep blood sugar levels within a target range and reduce the incidence of dizziness.
Symptoms of diabetes-related dizziness can vary from person to person but commonly include feeling light-headed, unsteady, or like you're about to faint. Some may also experience vertigo, a sensation that the room is spinning.
Other symptoms that can accompany dizziness include headaches, blurred vision, weakness, palpitations, and confusion. These symptoms can be particularly alarming when they occur suddenly, indicating the need for immediate action.
It's important for individuals with diabetes to be familiar with their own symptoms and to have a plan in place for when dizziness strikes. This includes having quick access to glucose sources, understanding when to seek medical help, and consistently managing diabetes to prevent such episodes.
Can High Blood Sugar Cause Vertigo?
While low blood sugar is often associated with dizziness, high blood sugar can also cause symptoms like vertigo. When blood sugar levels are too high, it can lead to a range of symptoms, including dizziness, due to the body’s response to excess glucose.
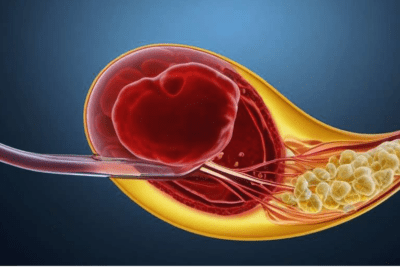
Dehydration resulting from high blood sugar can affect the vestibular system in the inner ear, which is responsible for balance. Moreover, prolonged periods of high blood sugar can lead to diabetic complications that affect blood flow and nerve function, further contributing to balance issues.
Managing blood sugar levels and maintaining good hydration are key to preventing these symptoms. If you're experiencing frequent vertigo, it's critical to discuss it with your healthcare provider to determine if it's related to your diabetes or if there's another underlying cause.
Frequently Asked Questions About Diabetes and Dizziness
What Does Diabetes Dizziness Feel Like?
For those with diabetes, dizziness can feel like a sudden onset of light-headedness, weakness, or a sensation of unsteadiness. This feeling is often accompanied by other symptoms such as sweating, shaking, and in severe cases, confusion or disorientation.
It's important to recognize these symptoms early on, as they can indicate fluctuations in blood sugar levels that need immediate attention. Managing diabetes effectively through diet, exercise, and medication is crucial in preventing such symptoms.
Why Do I Feel Weird Like Dizzy?
Feeling "weird" or dizzy can be caused by a range of factors, including low or high blood sugar levels, dehydration, certain medications, or even stress. For individuals with diabetes, it's essential to understand how these factors relate to their condition and to monitor blood sugar levels regularly.
If you're feeling dizzy and it's not related to blood sugar levels, consider other potential causes and consult with a healthcare provider for a thorough evaluation.
Does Prediabetes Make You Dizzy?
Prediabetes, a condition where blood sugar levels are elevated but not high enough to be classified as diabetes, can also lead to dizziness. This is particularly true if blood sugar levels fluctuate significantly, which can happen as the body struggles to regulate glucose.
Adopting lifestyle changes that can help stabilize blood sugar levels, such as a healthy diet and regular exercise, is important in managing prediabetes and preventing progression to type 2 diabetes.
Can High Blood Sugar Trigger Vertigo?
Yes, high blood sugar can trigger vertigo by affecting the body’s hydration status and the inner ear's balance system. If you have diabetes and experience vertigo, it's important to check your blood sugar levels and seek medical advice if the condition persists.
Managing diabetes is a comprehensive task that involves attention to diet, exercise, medication, and monitoring of blood sugar levels to prevent complications like vertigo.
In conclusion, diabetes management is a holistic approach that involves understanding and responding to symptoms like dizziness. By staying informed and prepared, those with diabetes can lead full and active lives.



