Diabetic retinopathy is a condition that affects the eyesight of those with diabetes, leading to potential vision loss. Regular monitoring of blood sugar levels and blood pressure is essential in preventing this complication.
With the rise of diabetes across the globe, understanding diabetic retinopathy—diabetes and eye problems is crucial for patients, caregivers, and healthcare providers. Let's delve into what this condition means for those affected and how best to manage it.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- What is diabetic retinopathy?
- Causes of diabetic retinopathy
- Symptoms of diabetic retinopathy
- Stages of diabetic retinopathy
- How is diabetic retinopathy diagnosed?
- Treatments for diabetic retinopathy
- How to prevent diabetic retinopathy
- Other eye problems related to diabetes
- Related questions about diabetic retinopathy and vision
What is diabetic retinopathy?
Diabetic retinopathy is an eye disease caused by high blood sugar levels damaging the blood vessels in the retina. Over time, this can result in blurred vision, floaters, and even total vision loss if not treated effectively.
It's a progressive condition that often begins without any noticeable symptoms but can escalate to more severe stages, affecting one's ability to perform daily tasks.
Proper management of diabetes is critical to delaying or preventing the onset of diabetic retinopathy, highlighting the importance of regular eye exams and diligent monitoring of blood glucose levels.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!









Causes of diabetic retinopathy
The primary cause of diabetic retinopathy is prolonged high blood sugar levels, which can damage the tiny blood vessels in the retina. This damage can lead to blockages, causing the blood vessels to leak or swell.
Other factors that may contribute to the development of this eye condition include high blood pressure, high cholesterol, and tobacco use. Understanding these causes is key to preventing or slowing down the progression of diabetic retinopathy.
The risk of developing diabetic retinopathy increases with the duration of diabetes, making longstanding diabetes a significant risk factor for this eye disease.
Symptoms of diabetic retinopathy
Initially, diabetic retinopathy may cause no symptoms or only mild vision problems. However, as the condition progresses, symptoms may include:
- Spots or dark strings floating in your vision (floaters)
- Blurriness
- Fluctuating vision
- Dark or empty areas in your vision
- Vision loss
It is essential for patients with diabetes to be aware of the symptoms of diabetic retinopathy and to seek medical advice if any changes in vision occur.
Stages of diabetic retinopathy
Diabetic retinopathy progresses through several stages, each with increasing severity:
- Mild Nonproliferative Retinopathy: Small areas of balloon-like swelling in the retina's blood vessels.
- Moderate Nonproliferative Retinopathy: Blood vessels that nourish the retina are blocked.
- Severe Nonproliferative Retinopathy: More blood vessels are blocked, leading to deprived areas of the retina, which signals the body to grow new blood vessels.
- Proliferative Retinopathy: The most advanced stage where the retina starts growing new blood vessels, which are fragile and can leak into the vitreous, potentially leading to serious vision problems.
Understanding these stages can help in early detection and treatment, potentially saving one's vision.
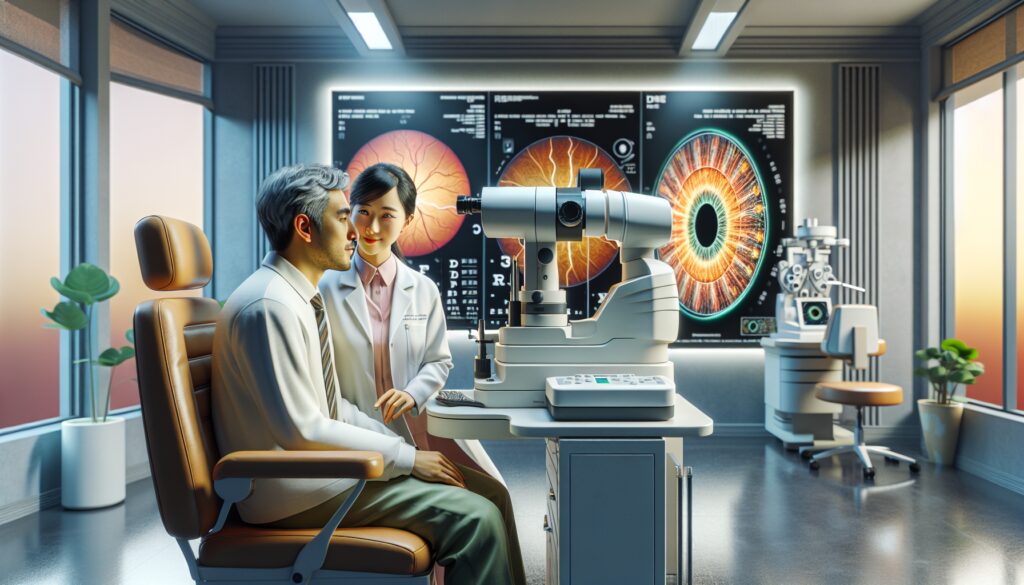
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed through a comprehensive dilated eye exam. During the exam, drops are placed in the eyes to widen the pupils, allowing the doctor to see more of the retina and look for signs of the disease.
Additional tests like fluorescein angiography and optical coherence tomography (OCT) may be used to gather more detailed images of the retina's structure and blood vessels.
Early diagnosis through regular screenings is crucial, as treatment is much more likely to be effective before significant vision loss has occurred.
Treatments for diabetic retinopathy
The treatment for diabetic retinopathy depends on the stage of the disease and the specific problems it has caused. Early-stage diabetic retinopathy may not require immediate treatment but will need to be monitored closely for changes.
Advanced diabetic retinopathy might require treatments such as:
- Laser treatment (photocoagulation)
- Injections of corticosteroids or anti-VEGF agents into the eye
- Vitrectomy surgery to remove blood from the middle of the eye
It's important to discuss the risks and benefits of these advanced diabetic retinopathy treatment options with an eye care specialist.
How to prevent diabetic retinopathy
To prevent or slow the progression of diabetic retinopathy, patients should focus on maintaining good blood sugar, blood pressure, and cholesterol levels. A healthy diet, regular exercise, and proper medication can all play a role in this effort.
Additionally, smoking cessation and careful management of blood glucose levels are critical preventive measures. Preventing diabetic retinopathy with regular eye exams is also a crucial step, as these exams can detect issues before they become severe.
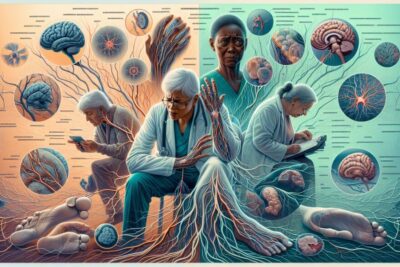
Diabetes can lead to other eye problems, such as diabetic macular edema (DME), glaucoma, and cataracts. Each of these conditions can cause vision impairment and requires different treatment approaches.
Regular eye check-ups can help detect these conditions early, allowing for timely intervention and better outcomes for those with diabetes.
How does diabetic retinopathy affect vision?
Diabetic retinopathy affects vision by damaging the blood vessels of the retina, leading to bleeding, swelling, and the formation of scar tissue. As the condition progresses, it can cause vision distortion and eventually blindness.
Maintaining blood sugar control is essential in mitigating these effects and preserving vision for individuals with diabetes.
What eye conditions are caused by diabetes?
Diabetes can cause several eye conditions, including diabetic retinopathy, diabetic macular edema, glaucoma, and cataracts. These conditions can all lead to significant vision impairment or loss if not managed properly.
Early detection and treatment are vital to prevent these diabetic eye problems from worsening.
How do you fix diabetic eye problems?
Diabetic eye problems can be managed with a combination of lifestyle changes, medication, and possibly surgical interventions. Laser treatment, anti-VEGF injections, and vitrectomy are among the options available for fixing severe diabetic eye problems.
Managing diabetic eye problems naturally also includes maintaining a healthy lifestyle with a balanced diet and regular exercise.
What are two symptoms of early stage diabetic retinopathy?
Early stage diabetic retinopathy may cause symptoms like mild blurriness and an increased number of floaters in one's vision. It's critical to report these symptoms to a healthcare professional as soon as they are noticed.
Regular monitoring and control of diabetes are vital in preventing these early symptoms from developing into more serious problems.
As we explore the complexities of diabetic retinopathy — diabetes and eye problems, it's clear that prevention through lifestyle management and regular screenings is paramount. For those looking for more information, this video offers additional insights:
By taking steps to control diabetes and scheduling regular eye exams, one can significantly reduce the risk of developing diabetic retinopathy and maintain healthy vision. Timely treatment and proactive prevention strategies are key to managing diabetic eye problems and ensuring the best possible outcomes.
✨ Other articles you might be interested in: