Diabetes is not just a condition that affects blood sugar levels; it can also have a significant impact on the skin. As many people with diabetes know, maintaining skin health is an important part of managing the overall condition.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- What Is Diabetes Mellitus?
- Common Skin Conditions Linked to Diabetes
- How Does Type 2 Diabetes Affect Skin Health?
- What Triggers Skin Diseases Associated With Diabetes?
- How Can Skin Diseases Associated With Diabetes Be Prevented?
- How Are Skin Diseases Treated?
- Exploring Diabetic Skin Complications: Further Questions
What Is Diabetes Mellitus?
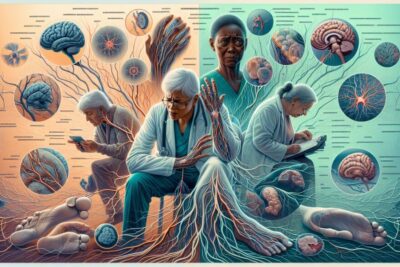
Diabetes mellitus is a chronic condition where the body either doesn't produce enough insulin or can't effectively use the insulin it does produce. This can lead to high levels of sugar in the blood, which over time can damage various parts of the body, including the skin.
For those living with diabetes, it's crucial to understand the connection between high blood glucose levels and skin complications. High blood sugar can cause dehydration and dry skin, which can crack and allow bacteria to enter, potentially leading to infections.
Diabetes can cause changes in small blood vessels, which can lead to skin problems as well. Moreover, nerve damage from diabetes can cause sweating abnormalities that affect skin moisture levels.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!










Common Skin Conditions Linked to Diabetes
Diabetes can lead to a range of skin conditions, some of which are more common in those with diabetes than in the general population. For example, diabetic dermopathy, which appears as light brown, scaly patches, often on the legs, is seen in many diabetic patients.
Bacterial infections such as styes, boils, and carbuncles are more frequent in diabetic individuals. Similarly, fungal infections, like athlete's foot and ringworm, thrive when sugar levels are high.
Other conditions include necrobiosis lipoidica diabeticorum, which causes raised, hard patches on the skin, and eruptive xanthomatosis, which can cause firm, yellow, pea-like enlargements in the skin.
With around 30% of individuals with diabetes experiencing skin problems, it’s evident that diabetic skin care should be a priority.
How Does Type 2 Diabetes Affect Skin Health?
Type 2 diabetes, which is characterized by insulin resistance, can have a significant impact on skin health. Persistent high blood sugar can lead to poor circulation and reduced blood flow to the skin, which impairs its ability to heal and increases susceptibility to infections.
Moreover, those with type 2 diabetes may experience diabetic blisters, which are rare but can occur on the hands, feet, and forearms. These blisters might look alarming, but they're usually painless and heal on their own.
It's important for individuals with type 2 diabetes to manage their blood sugar levels and maintain a healthy diet to prevent skin complications.
What Triggers Skin Diseases Associated With Diabetes?
Several factors can trigger skin diseases in individuals with diabetes. Poor blood glucose control is a major trigger, as it can lead to the dry and cracked skin that invites pathogens. Additionally, poor circulation and the reduced ability to fight off infections can exacerbate skin conditions.
Environmental factors, such as hot or cold weather, can also affect the skin's health, making it more prone to complications. And not to forget, the pre-existing genetic predisposition to certain skin conditions can be a potent trigger as well.
How Can Skin Diseases Associated With Diabetes Be Prevented?
Prevention is key when it comes to diabetes and skin complications. Regular monitoring of blood sugar levels and maintaining them within a healthy range is the most important step.
Additionally, daily skin care routines, including the use of mild shampoos, moisturizers, and careful foot care, can reduce the risk of developing skin issues.
Patients should be educated on the importance of regular skin checks and consulting a healthcare provider when they notice any changes in their skin. Wearing proper footwear and avoiding extreme temperatures can also help.
How Are Skin Diseases Treated?
Treatment for diabetic skin conditions can vary based on the specific issue. Topical agents and emollients are often used to treat dry skin and prevent infections. For fungal infections, antifungal creams and medications may be prescribed.
For more serious conditions, like necrobiosis lipoidica diabeticorum, corticosteroid injections or other treatments may be necessary. Urea-based creams are often recommended for foot care to manage calluses and prevent ulcers.
Regular visits to a dermatologist can help manage existing skin problems and prevent new ones from developing. It’s essential for individuals with diabetes to receive comprehensive care that includes skin management.
Exploring Diabetic Skin Complications: Further Questions
What Does Diabetic Dermatitis Look Like?
Diabetic dermatitis often appears as itchy, red rashes with bumps that can sometimes ooze fluid. It's typically found in areas where the skin folds and can come along with a fungal infection known as Candida albicans.
Proper hygiene and the use of topical steroids or antifungal creams are common approaches to treatment. It is important to consult a healthcare provider for an accurate diagnosis and treatment plan.
What Three Drinks Should Diabetics Avoid?
Diabetics are advised to avoid sugary drinks like sodas, fruit juices with added sugars, and energy drinks. These can cause blood glucose levels to spike, negatively affecting diabetes management and potentially leading to skin complications amongst other health issues.
Instead, water, unsweetened tea, and black coffee are better choices that help maintain hydration without impacting blood sugar levels.
What Does Diabetes Burnout Look Like?
Diabetes burnout can take a toll on mental and physical health. It often presents as feelings of frustration, defeat, or being overwhelmed by the constant vigilance required to manage diabetes.
It's essential to address these feelings by seeking support from a healthcare team, family, friends, or support groups. Taking breaks from strict management routines, without neglecting overall health, can also help.
How Do You Treat a Diabetic Skin Infection?
The treatment for a diabetic skin infection typically includes antibiotics for bacterial infections or antifungal medications for fungal infections. It's important to keep the affected area clean and dry and to follow the treatment regimen prescribed by a healthcare provider.
Preventing infections by managing diabetes effectively and practicing good skin care is crucial.
Understanding and managing diabetes and skin complications involves a comprehensive approach that addresses both blood sugar control and skin care. Keeping the skin healthy is an integral part of diabetes management and can go a long way in preventing serious complications.
Let's take a moment to learn more from a healthcare expert on this topic. Below is an informative video that discusses the best practices for diabetic skin care:
In summary, managing diabetes-related skin issues requires an understanding of the risks, preventative measures, and treatments. Regular consultations with healthcare providers, adherence to diabetes management plans, and routine skin care can help mitigate the chances of developing skin complications. By staying informed and proactive, individuals with diabetes can maintain not only their overall health but also the health of their skin.
✨ Other articles you might be interested in:
- Navigating Commercial Driving and Diabetes: What You Need to Know
- Understanding Diabetes and Pregnancy | ADA Guidelines
- Exploring the Pathophysiological Impact of Nevro HFX™ High-Frequency (10 kHz) Spinal Cord Stimulation for Painful Diabetic Neuropathy
- Hypoglycemia emergency care plan for low blood glucose situations
- Understanding diabetes and emotional health challenges



