
Living with diabetes can be challenging, not only because of the physical care required but also due to the emotional toll it can take. This emotional response, known as diabetes distress, can significantly impact an individual's quality of life and diabetes management. In this guide, we'll explore diabetes distress, its symptoms, causes, and solutions to effectively cope with this common but often unaddressed aspect of diabetes care.
Recognizing and managing diabetes distress is a critical component of comprehensive diabetes care. By understanding how emotional well-being is interwoven with physical health, individuals with diabetes can take proactive steps to improve their overall health and well-being. Let's delve into the various facets of diabetes distress and discover strategies to enhance emotional health.
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!
What you\'ll find in this article?
- What is diabetes distress?
- How can I identify diabetes distress?
- Symptoms of diabetes distress
- Diabetes distress vs. depression
- Coping strategies for diabetes distress
- The role of family support in diabetes distress
- Using the PAID scale to measure diabetes distress
- Diabetes distress and glycemic control
- Understanding chapter 3 - diabetes distress: Questions related to coping strategies
What is diabetes distress?
Diabetes distress refers to the unique, often hidden emotional burden that comes with the day-to-day management of diabetes. It encompasses the worries, fears, and frustrations associated with managing a chronic condition that demands constant vigilance and self-care. Unlike clinical depression, diabetes distress is directly related to the demands of diabetes management and can fluctuate as these demands change.
Understanding that diabetes distress is a common experience can be reassuring for those who might feel isolated in their struggles. It's crucial to acknowledge that these feelings are a normal response to a challenging situation and to seek appropriate support to mitigate their impact.
As a comprehensive resource for how to cure diabetes, we aim to equip you with the knowledge and tools to address not only the physical aspects of diabetes but also the emotional challenges that accompany it.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!

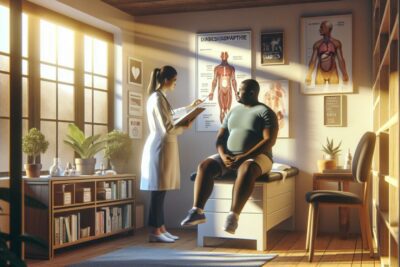






How can I identify diabetes distress?
Identifying diabetes distress involves being mindful of changes in emotions and behaviors that could indicate a struggle with the psychological demands of diabetes management. Some signs to watch for include:
- Feeling overwhelmed by diabetes care routines
- Experiencing feelings of guilt or failure related to diabetes management
- Worrying excessively about potential complications
- Feeling angry or resentful about having diabetes
- Withdrawing from social activities or neglecting self-care due to diabetes-related stress
Recognizing these signs early can lead to timely interventions that prevent diabetes distress from escalating and negatively affecting glycemic control and quality of life.
It's essential to conduct a self-assessment and seek professional help if you notice persistent distress that interferes with your daily life. Remember, addressing emotional health is just as important as managing blood glucose levels.
Symptoms of diabetes distress
Symptoms of diabetes distress might manifest in various ways, and it's important to differentiate them from the clinical symptoms of depression. Common symptoms include:
- Constant concerns about not managing diabetes well enough
- Avoiding healthcare appointments or blood glucose monitoring
- Feeling powerless or defeated by the diabetes care regimen
- Experiencing mood swings or irritability without an apparent cause
- Changes in appetite, sleep patterns, or energy levels related to diabetes management stress
By being attentive to these symptoms, individuals with diabetes can take steps to seek support and implement coping strategies before distress becomes overwhelming.
Diabetes distress vs. depression
While diabetes distress and depression can share similar symptoms, they are distinct conditions. Diabetes distress is specifically related to the emotional burden of managing diabetes, while depression is a clinical mental health condition that affects various aspects of life, not just those related to diabetes.
Understanding the difference is key to seeking the right kind of help. Depression may require treatment such as medication or therapy, whereas diabetes distress might be alleviated through targeted support and diabetes education.
It's important to consult with a healthcare professional to accurately diagnose and treat either condition. Early detection and intervention can prevent further emotional deterioration and improve overall health outcomes.
Coping strategies for diabetes distress
Coping with diabetes distress involves a combination of self-care practices and professional support. Here are some strategies that can help:
- Engage in regular physical activity to reduce stress and improve mood.
- Adopt a balanced diet that supports overall health and glycemic control.
- Practice self-compassion and give yourself credit for managing a complex condition.
- Set realistic goals for diabetes management to avoid feeling overwhelmed.
- Seek support from friends, family, or diabetes support groups to share experiences and tips.
Additionally, consider mindfulness or stress-reduction techniques such as meditation or yoga, which can help alleviate the emotional burden of diabetes.
Professional counseling or therapy may also be beneficial, especially if distress is significantly impacting your quality of life. Remember, seeking help is a sign of strength and an important step in managing your diabetes effectively.
The role of family support in diabetes distress
Family support plays a crucial role in managing diabetes distress. Having a strong support system can provide emotional comfort, practical assistance, and motivation to maintain good diabetes management practices.
Encourage open communication with family members about the challenges and needs related to your diabetes care. Educating them about diabetes can also help them understand your situation better and provide more effective support.
Remember, support from loved ones can make a significant difference in reducing feelings of isolation and boosting morale when coping with diabetes distress.
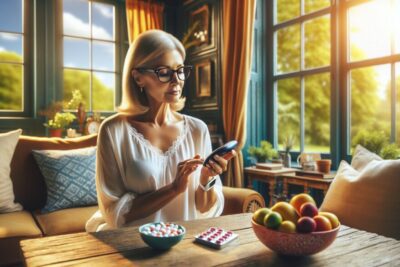
Using the PAID scale to measure diabetes distress
The Problem Areas in Diabetes (PAID) scale is a validated tool used to measure diabetes distress levels. It consists of a questionnaire that assesses emotional responses related to diabetes self-care, treatment, and complications.
Utilizing the PAID scale can help individuals and healthcare providers identify areas of concern and tailor interventions to address specific challenges. Regular use of the PAID scale can also track changes in distress over time, providing valuable insights into the effectiveness of coping strategies.
If you're experiencing diabetes distress, consider discussing the PAID scale with your healthcare provider to gain a clearer understanding of your emotional well-being.
Diabetes distress and glycemic control
Research has shown a connection between diabetes distress and glycemic control. High levels of distress can negatively impact self-care behaviors, leading to suboptimal blood glucose levels and an increased risk of complications.
Addressing diabetes distress is therefore not only important for improving emotional health but also for maintaining good glycemic control. Collaborative care that includes emotional support can enhance diabetes self-management and contribute to better health outcomes.
It's vital to recognize the interconnectedness of emotional and physical health in diabetes care and to approach management with a holistic perspective.
What is the paid score for diabetes distress?
The PAID score is a numerical value derived from the PAID scale, which assesses various aspects of emotional distress in individuals with diabetes. A high PAID score indicates a higher level of distress, which may necessitate intervention through counseling, support groups, or changes in diabetes management strategies.
Regular monitoring of the PAID score can help individuals and healthcare professionals track progress in managing emotional health and make necessary adjustments to treatment plans.
What is the difference between diabetes distress and diabetes burnout?
Diabetes distress refers to the emotional burden specifically related to managing diabetes, while diabetes burnout is characterized by a state of physical or emotional exhaustion resulting from the relentless demands of diabetes care. Burnout can lead to a reduction in or cessation of diabetes self-care activities.
Understanding the distinction between these two experiences is essential for implementing appropriate coping mechanisms and seeking professional support when needed.
What is the distress scale for diabetes?
The distress scale for diabetes, commonly known as the PAID scale, is a questionnaire that individuals can use to express their feelings about diabetes management and its impact on their lives. The scale helps quantify the distress level, allowing for targeted interventions.
Healthcare providers often use this scale during consultations to gauge the emotional state of their patients and to address any concerns that may arise from the emotional burden of diabetes.
What is the 7 as model for diabetes distress?
The 7 As model for diabetes distress is an approach that includes seven components: Acknowledge, Assess, Accept, Articulate, Assist, Act, and Adjust. It provides a framework for understanding and addressing the emotional aspects of diabetes management.
Utilizing this model can help individuals with diabetes and healthcare professionals work collaboratively to identify distress and develop effective strategies to cope with the challenges of diabetes care.
Emotional health is an integral part of diabetes management. By addressing diabetes distress proactively, individuals can improve their quality of life and successfully manage their condition. If you're struggling with diabetes-related emotional issues, remember that support is available, and taking steps to address your emotional well-being is a critical part of your health journey.
✨ Other articles you might be interested in:



