Medical Conditions Diabetes: Identifying & Managing

Medical conditions diabetes refers to a group of chronic conditions that affect how the body processes and regulates blood sugar. There are three main types: type 1, type 2, and gestational diabetes. Symptoms may include increased thirst, frequent urination, unexplained weight loss, fatigue, and slow wound healing. Managing diabetes involves maintaining a healthy lifestyle, monitoring blood sugar levels regularly, and seeking appropriate treatment options. This article provides an overview of diabetes types, symptoms, management strategies, and the importance of education and support.
- Types of Diabetes
- Understanding the Symptoms of Diabetes - Medical Conditions Diabetes: Identifying & Managing
-
Managing Diabetes: Diet and Lifestyle - Medical Conditions Diabetes: Identifying & Managing
- Introduction to Diabetes Management
- Importance of a Balanced Diet
- The Role of Physical Activity in Diabetes Management
- Carbohydrate Intake and Blood Glucose Control
- Strategic Meal Planning for Blood Sugar Stability
- Navigating Weight Management in Diabetes Care
- Mitigating Stress for Optimal Health
- Conclusion: Holistic Strategies for Effective Diabetes Management
- Importance of Regular Blood Sugar Monitoring - Medical Conditions Diabetes: Identifying & Managing
- Treatment Options for Diabetes - Medical Conditions Diabetes: Identifying & Managing
- Preventing Type 2 Diabetes: Risk Factors and Prevention - Medical Conditions Diabetes: Identifying & Managing
- Diabetes and Kidney Disease - Medical Conditions Diabetes: Identifying & Managing
- Diabetes and Heart Disease - Medical Conditions Diabetes: Identifying & Managing
- Living with Diabetes: Education and Support - Medical Conditions Diabetes: Identifying & Managing
- Frequently Asked Questions (FAQs) about Diabetes
Types of Diabetes
Diabetes is a complex condition with different types that affect individuals in distinct ways. Understanding the types of diabetes can help in managing and treating the condition effectively.
Type 1 Diabetes
Type 1 diabetes, also known as juvenile diabetes, typically develops in childhood or adolescence. It occurs when the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. Individuals with type 1 diabetes require insulin therapy to regulate their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes, the most common type, occurs when the body becomes resistant to insulin or fails to produce enough insulin to maintain normal blood sugar levels. It often develops in adults over the age of 40, but due to increasing rates of obesity, it is also affecting younger individuals. Lifestyle changes, such as adopting a healthy diet and regular exercise, along with medication, may be necessary to manage type 2 diabetes.
Gestational Diabetes
Gestational diabetes occurs during pregnancy in women who have never had diabetes before. Hormonal changes during pregnancy can lead to insulin resistance, resulting in high blood sugar levels. It is essential to monitor and manage gestational diabetes to ensure the health of both the mother and baby. In most cases, blood sugar levels return to normal after delivery.
Understanding the Symptoms of Diabetes - Medical Conditions Diabetes: Identifying & Managing
Diabetes is characterized by various symptoms that can indicate the presence of the condition. Recognizing these symptoms is crucial for early diagnosis and timely management. Here are some key symptoms to be aware of:
- Excessive thirst: Individuals with diabetes often experience persistent thirst and increased fluid intake.
- Frequent urination: A common symptom of diabetes is frequent urination, as the body tries to eliminate excess glucose through urine.
- Unexplained weight loss: Sudden weight loss can occur with diabetes, as the body is unable to effectively utilize glucose for energy.
- Fatigue: Feeling excessively tired or fatigued, even after adequate rest, is a symptom associated with diabetes.
- Blurred vision: Elevated blood sugar levels can cause temporary changes in vision, resulting in blurred vision.
- Slow wound healing: Diabetes can impact the body's ability to heal wounds and injuries due to impaired blood circulation.
- Recurrent infections: Individuals with diabetes may be prone to frequent infections, particularly urinary tract infections and skin infections.
If you experience any of these symptoms, it is important to consult a healthcare professional for evaluation and possible diagnosis of diabetes. Prompt identification and treatment can help prevent complications and promote overall wellness.
Managing Diabetes: Diet and Lifestyle - Medical Conditions Diabetes: Identifying & Managing
Introduction to Diabetes Management
Managing diabetes involves making significant changes to one's diet and lifestyle to maintain stable blood sugar levels and support overall health. Here are some key strategies:
Importance of a Balanced Diet
Healthy Eating: Adopting a balanced and nutritious diet is essential for managing diabetes. This includes consuming a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. It's important to monitor portion sizes and limit the intake of sugary and processed foods that can spike blood sugar levels.
The Role of Physical Activity in Diabetes Management
Regular Physical Activity: Engaging in regular exercise offers various benefits for individuals with diabetes. Physical activity helps to lower blood sugar levels, improve insulin sensitivity, manage weight, and boost overall well-being. Incorporating activities like brisk walking, cycling, swimming, or strength training into daily routines can be highly beneficial.
Carbohydrate Intake and Blood Glucose Control
Monitoring Carbohydrate Intake: Carbohydrates directly affect blood glucose levels, so individuals with diabetes should carefully monitor their carbohydrate intake. Understanding the concept of glycemic index and glycemic load can help in choosing foods that have a lesser impact on blood sugar levels.
Strategic Meal Planning for Blood Sugar Stability
Frequent Meal Planning: Consistent meal planning is essential for maintaining stable blood sugar levels. This involves spreading meals throughout the day, consuming regular snacks, and avoiding long periods without eating. Meal planning can help individuals make healthier food choices and effectively manage portion sizes.
Weight Management: Achieving and maintaining a healthy weight plays a crucial role in diabetes management. Losing excess weight can improve insulin sensitivity and blood sugar control. Working with a healthcare professional or registered dietitian can provide guidance on setting realistic weight loss goals and developing a personalized plan.
Mitigating Stress for Optimal Health
Stress Management: Stress can impact blood sugar levels and overall well-being. Engaging in stress-reducing activities like meditation, deep breathing exercises, and pursuing hobbies or activities that bring joy and relaxation can contribute to better diabetes management.
Conclusion: Holistic Strategies for Effective Diabetes Management
By proactively managing diabetes through a combination of healthy eating, regular physical activity, and other lifestyle modifications, individuals can maintain better control over their blood sugar levels and reduce the risk of complications associated with the condition.
Importance of Regular Blood Sugar Monitoring - Medical Conditions Diabetes: Identifying & Managing
Regular blood sugar monitoring plays a crucial role in managing diabetes effectively. By monitoring your blood sugar levels, you can gain valuable insights into how your body processes glucose and make informed decisions about your daily management routine. Here are some key reasons why regular blood sugar monitoring is essential:
- Understanding your body's response: Monitoring blood sugar levels helps you understand how your body reacts to different foods, medications, and activities. It enables you to identify patterns and make necessary adjustments to maintain stable blood sugar levels.
- Preventing complications: Consistent monitoring enables early detection of high or low blood sugar levels, reducing the risk of short-term complications such as hypoglycemia and hyperglycemia.
- Improving treatment effectiveness: Monitoring allows you to assess the effectiveness of your diabetes management plan, including medications, diet, exercise, and lifestyle changes. If your blood sugar levels consistently fall outside the target range, you can work with your healthcare team to adjust your treatment accordingly.
- Empowering self-care: Regular monitoring empowers individuals with diabetes to take control of their health. It provides valuable information for making informed decisions about meals, physical activity, and medication doses.
Remember, blood sugar levels can fluctuate throughout the day, so it's essential to monitor regularly. Consult with your healthcare team to determine the frequency and timing of blood sugar checks that align with your specific needs. By actively monitoring your blood sugar levels, you can take proactive steps toward effectively managing your diabetes and reducing the risk of long-term complications.
Treatment Options for Diabetes - Medical Conditions Diabetes: Identifying & Managing
When it comes to managing diabetes, there are various treatment options available that can help individuals maintain stable blood sugar levels and prevent complications. The specific treatment approach depends on the type of diabetes and its severity. Here are some common treatment options:
- Insulin therapy: For individuals with type 1 diabetes or advanced type 2 diabetes, insulin therapy may be necessary. This involves injecting insulin into the body to regulate blood sugar levels.
- Oral medications: Type 2 diabetes can often be managed with oral medications that help the body use insulin more effectively or reduce glucose production in the liver.
- Dietary changes: Following a healthy eating plan tailored to diabetes management is crucial. This includes controlling portion sizes, monitoring carbohydrate intake, and focusing on whole grains, lean proteins, and fruits and vegetables.
- Regular physical activity: Engaging in regular exercise can help improve insulin sensitivity and lower blood sugar. It's recommended to aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Continuous glucose monitoring (CGM): CGM devices can track blood sugar levels in real-time, allowing individuals to make informed decisions about insulin dosing and lifestyle adjustments.
- Education and support: Diabetes self-management education programs provide valuable knowledge and resources to individuals living with diabetes. Support from healthcare professionals and peer groups can also be beneficial.
It's important to work closely with healthcare professionals to develop a personalized treatment plan that meets individual needs and goals. Regular monitoring and adjustments may be necessary to maintain optimal blood sugar control and reduce the risk of complications associated with diabetes.
Preventing Type 2 Diabetes: Risk Factors and Prevention - Medical Conditions Diabetes: Identifying & Managing
Preventing type 2 diabetes involves understanding the risk factors and taking proactive steps towards prevention. While some factors, such as age and genetics, are beyond our control, there are lifestyle changes that can significantly reduce the risk.
Here are some key factors to consider:
- Healthy Weight: Maintaining a healthy weight through a balanced diet and regular physical activity can lower the risk of type 2 diabetes.
- Dietary Choices: Choosing nutrient-rich foods, limiting processed sugars and carbohydrates, and incorporating plenty of fruits, vegetables, whole grains, and lean proteins can promote better blood sugar control.
- Physical Activity: Engaging in regular exercise, such as brisk walking, cycling, or swimming, can help improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
- Smoking and Alcohol: Quitting smoking and moderating alcohol intake are essential for reducing the risk of various health conditions, including type 2 diabetes.
- Regular Check-ups: Regular medical check-ups, including blood sugar tests, can help monitor any changes and detect prediabetes or early signs of diabetes.
By taking preventive measures and adopting a healthy lifestyle, individuals can greatly reduce their risk of developing type 2 diabetes. It is important to consult with healthcare professionals for personalized guidance and support in managing and preventing this condition.
Diabetes and Kidney Disease - Medical Conditions Diabetes: Identifying & Managing
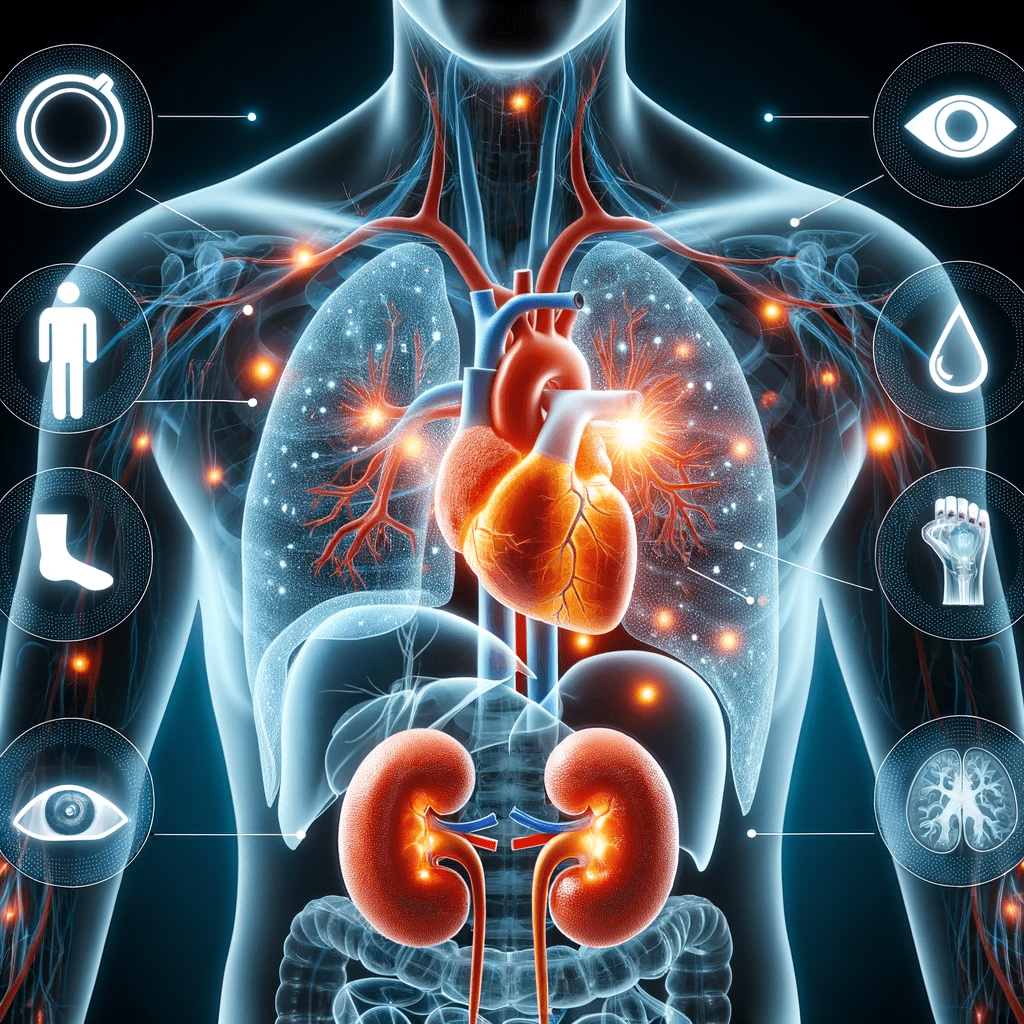
Diabetes increases the risk of developing kidney disease, also known as diabetic nephropathy. When blood sugar levels are consistently high, it can damage the small blood vessels and filters in the kidneys.
Over time, this can lead to reduced kidney function and even kidney failure. It is estimated that diabetes is the leading cause of kidney failure in the United States. Fortunately, there are steps individuals with diabetes can take to reduce the risk of kidney disease.
Managing diabetes is crucial in preventing kidney complications. This involves maintaining tight control of blood sugar levels through medication, lifestyle modifications, and regular blood sugar monitoring.
Additionally, controlling blood pressure is equally important as high blood pressure can further damage the kidneys. Doctors may prescribe medications to manage blood pressure and may recommend dietary changes, such as reducing salt intake, to help maintain healthy blood pressure levels.
Regular check-ups with healthcare providers are essential in monitoring kidney health. They may conduct urine tests to detect any signs of kidney damage and order blood tests to assess kidney function.
By effectively managing diabetes and taking steps to protect kidney health, individuals can significantly reduce the risk of developing diabetic kidney disease and the need for dialysis or kidney transplant in the future.
Diabetes and Heart Disease - Medical Conditions Diabetes: Identifying & Managing
People with diabetes are at an increased risk of developing heart disease. The relationship between diabetes and heart disease is complex and multifactorial. High levels of blood sugar over time can lead to the buildup of fatty deposits in the arteries, known as atherosclerosis, which can restrict blood flow to the heart. This increases the risk of heart attacks, strokes, and other cardiovascular complications.
Managing diabetes is crucial in reducing the risk of heart disease. It involves maintaining healthy blood sugar levels, controlling blood pressure and cholesterol, and adopting a heart-healthy lifestyle. A balanced diet, regular exercise, not smoking, and managing stress are essential components of managing diabetes and preventing heart disease.
Regular medical check-ups and screenings are important for individuals with diabetes to assess their heart health. These may include tests to monitor blood pressure, cholesterol levels, and heart function. Medications may be prescribed to control blood pressure and cholesterol, and aspirin therapy may be recommended to reduce the risk of blood clotting.
Education and support play a vital role in managing diabetes and preventing heart disease. Individuals with diabetes should be knowledgeable about their condition, understand the connection to heart health, and work closely with their healthcare team to develop a personalized management plan. By managing diabetes effectively, individuals can significantly reduce the risk of heart disease and maintain a healthier heart.
Living with Diabetes: Education and Support - Medical Conditions Diabetes: Identifying & Managing
When it comes to managing diabetes, education and support play a crucial role in helping individuals live a healthy and fulfilling life. Here are some key aspects to consider:
- Understanding the condition: Learning about diabetes, its types, causes, and potential complications is essential. Educate yourself on how to monitor blood sugar levels, recognize symptoms, and manage the condition effectively.
- Dietary guidance: Work with a registered dietitian to create a personalized meal plan that balances blood sugar levels, incorporates nutrient-rich foods, and helps with weight management.
- Lifestyle modifications: Regular physical activity is beneficial for managing diabetes. Consult with a healthcare professional to develop an exercise routine that suits your abilities and preferences.
- Medication adherence: Take medications as prescribed by your healthcare provider, following the recommended schedule and dosage. Keep track of any side effects and report them to your doctor.
- Emotional support: Living with diabetes can be challenging emotionally. Seek support from family, friends, or join support groups to connect with others facing similar experiences.
- Continuous learning: Stay up to date with the latest research, advancements, and treatment options for diabetes. Attend educational workshops, seminars, or online resources to expand your knowledge.
Remember, diabetes management is a lifelong journey, but with the right education, support, and self-care, individuals with diabetes can lead a fulfilling life and reduce the risk of complications.
Frequently Asked Questions (FAQs) about Diabetes
- What are the different types of diabetes?
- What are the common symptoms of diabetes?
- How can diabetes be managed?
- What are the risks associated with diabetes?
- How can type 2 diabetes be prevented?
Preventing type 2 diabetes involves maintaining a healthy weight, making nutritious food choices, engaging in regular physical activity, and managing prediabetes. It is important to be aware of risk factors like family history, genetics, race or ethnicity, and overweight or obesity.