
Diabetes Type 2 can be effectively managed and even reversed through key lifestyle changes. These changes include weight loss and exercise, as studies have shown their positive impact on blood sugar control. Low-calorie diets have also proven beneficial in achieving diabetes remission. Bariatric surgery is an option for weight loss and reversing diabetes. This article explores strategies for achieving remission, long-term management techniques, and answers common questions about Diabetes Type 2. Taking early action and adopting a healthy lifestyle is crucial in preventing complications. How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
🔍 Seeking a breakthrough in Type 2 Diabetes management?
Discover our expert insights and innovative approaches on ‘How to Cure Diabetes’.
Click to transform your health journey today!

What you\'ll find in this article?
- Understanding Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
- Managing Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
- Reversing Diabetes Type 2: Key Strategies - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
- Living with Remission: Long-Term Strategies - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
-
Frequently Asked Questions about Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
- Is it possible to permanently cure Diabetes Type 2?
- How can weight loss help in remission?
- Are there natural therapies for diabetes reversal?
- What role does medication play in remission?
- Can exercise alone reverse Diabetes Type 2?
- Is bariatric surgery a recommended option?
- How important is early diagnosis and intervention?
- Is achieving remission without medication possible?
- What are the potential complications of Diabetes Type 2?
- Where can I find additional support and resources?
Understanding Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
High blood sugar levels due to ineffective use of insulin characterize Diabetes Type 2, a chronic metabolic disorder. Unlike Type 1 diabetes, lifestyle factors often associate with it, and it typically develops later in life. Understanding the key aspects of this condition is crucial for effective management and potential remission.
What is Diabetes Type 2?
Diabetes Type 2 occurs when the body becomes resistant to insulin or doesn't produce enough insulin to regulate blood sugar levels adequately. Insulin is a hormone that helps glucose enter cells to provide energy. When the body struggles to utilize insulin effectively, blood sugar levels increase, leading to various health complications over time.
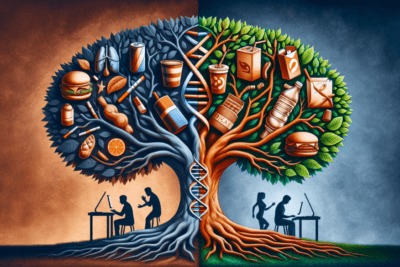
Causes and Risk Factors
Several factors contribute to the development of Type 2 diabetes, including genetics, sedentary lifestyle, obesity, and poor dietary choices. People with a family history of diabetes, a sedentary lifestyle, or who are overweight are more likely to develop Type 2 diabetes. Additionally, certain ethnic groups, such as African Americans, Hispanic Americans, and Native Americans, are at higher risk.
Diagnosis and Symptoms
Diagnosing Type 2 diabetes involves several tests, including blood glucose tests, A1C tests, and oral glucose tolerance tests. Common symptoms of diabetes Type 2 include increased thirst, frequent urination, unexplained weight loss or gain, fatigue, blurred vision, and slow-healing sores. However, some individuals may have diabetes without experiencing noticeable symptoms.
Explore our specialized services in diabetes care 🌟.
From personalized diet plans to effective exercise routines, we have what you need to take control of Type 2 Diabetes.
Visit our services page now!



Managing Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
Proper management of Type 2 diabetes is essential for maintaining optimal health and preventing complications. This section focuses on important aspects of managing the condition effectively.
Medication and Insulin Therapy
For many individuals with Type 2 diabetes, medication and insulin therapy play a vital role in controlling blood sugar levels. Depending on the severity of the condition, healthcare providers may prescribe oral medications, injectable insulin, or a combination of both. It is crucial to follow the prescribed medication regimen carefully and regularly monitor blood sugar levels to ensure they remain within the target range.
Blood Sugar Monitoring
Regular monitoring of blood sugar levels is essential for individuals with Type 2 diabetes. This helps in understanding how certain foods, physical activity, and medication affect blood sugar levels. Blood glucose monitoring devices, such as glucometers, allow individuals to measure their blood sugar levels at home. Healthcare providers can guide on the frequency and timing of monitoring based on individual needs.
Importance of Lifestyle Changes
Lifestyle changes play a significant role in managing and improving Type 2 diabetes. Making healthy choices regarding diet, physical activity, and overall lifestyle can help control blood sugar levels and potentially lead to remission. Experts recommend a balanced diet rich in whole grains, lean proteins, fruits, and vegetables. Regular physical activity, such as brisk walking or aerobic exercises, helps in maintaining a healthy weight and improving insulin sensitivity.
Furthermore, adopting healthy habits like quitting smoking, reducing alcohol consumption, and managing stress levels can have a positive impact on diabetes management. It is important to work closely with healthcare providers to develop an individualized plan that addresses specific needs and goals.
By effectively managing Type 2 diabetes through medication, blood sugar monitoring, and lifestyle changes, individuals can reduce the risk of complications and enhance their overall well-being.
Reversing Diabetes Type 2: Key Strategies - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission

Reversing diabetes type 2 requires a comprehensive approach that focuses on key strategies to achieve remission. By implementing these strategies, individuals with type 2 diabetes can potentially normalize their blood sugar levels and reduce their dependency on medication.
Weight Loss and Diabetes Remission
One of the most crucial steps in reversing diabetes type 2 is weight loss. Research has consistently shown that losing as little as 5% to 10% of body weight can significantly improve insulin sensitivity and glucose control. This can lead to a state of remission, where blood sugar levels remain within the normal range without the need for medication.
Adopting a combination of a calorie-restricted diet and regular physical activity is essential for successful weight loss. By reducing calorie intake and increasing energy expenditure through exercise, individuals can effectively achieve weight loss and improve their chances of reversing type 2 diabetes.
Low-Calorie Diets and Blood Sugar Control
A very low-calorie diet, usually consisting of around 800 to 1,200 calories per day, has shown promising results in reversing diabetes type 2. This type of diet promotes weight loss and helps control blood sugar levels. Medical professionals often recommend it under supervision to ensure proper nutrition and monitor potential side effects.
Low-calorie diets typically focus on reducing carbohydrates and increasing the intake of lean proteins, healthy fats, and fiber-rich foods. By carefully managing portion sizes and making smart food choices, individuals can achieve better blood sugar control and potentially reverse their diabetes.
The Role of Exercise in Remission
A regular exercise routine plays a significant role in reversing diabetes type 2. Physical activity helps lower blood sugar levels by improving insulin sensitivity and promoting weight loss. It also helps maintain cardiovascular health and overall well-being.
Engaging in both aerobic exercises, such as walking, jogging, or cycling, and strength training activities can provide remarkable benefits for individuals with type 2 diabetes. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with two or more days of strength training exercises.
Bariatric Surgery and Diabetes Reversal
Individuals with diabetes type 2 who have a body mass index (BMI) above a certain threshold consider bariatric surgery as an option. This surgical procedure helps achieve significant weight loss, which can result in remission of diabetes.
While bariatric surgery can be highly effective in reversing diabetes, it is important to understand that it is not a guaranteed solution and requires careful consideration. Individuals should consult with healthcare professionals to make the decision to undergo bariatric surgery, considering individual circumstances and potential risks.
- Weight loss is a key strategy in reversing diabetes type 2.
- A low-calorie diet can help control blood sugar levels.
- Regular exercise improves insulin sensitivity and promotes weight loss.
- Bariatric surgery may be an option for weight loss and diabetes reversal.
Living with Remission: Long-Term Strategies - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission
Maintaining a Healthy Diet
One of the key components of successfully living with diabetes Type 2 remission is maintaining a healthy diet. This means consuming a well-balanced meal plan that is rich in fruits, vegetables, whole grains, and lean proteins. Avoiding processed foods, sugary beverages, and excessive saturated fats is crucial for long-term success. It's important to consult with a registered dietitian to create a personalized meal plan that meets your specific needs and helps you sustain remission.
Regular Physical Activity
Incorporating regular physical activity into your daily routine is another essential aspect of living with diabetes Type 2 remission. Engaging in at least 150 minutes of moderate-intensity aerobic exercise, such as brisk walking or swimming, along with muscle-strengthening activities two or more days a week, can help maintain a healthy weight and improve insulin sensitivity. It's important to find physical activities that you enjoy and make them a regular part of your lifestyle.
Monitoring Blood Sugar Levels
Even in remission, it's vital to monitor your blood sugar levels regularly. Individuals can achieve this through self-monitoring using a glucose meter or continuous glucose monitoring (CGM) devices. By keeping track of your blood sugar levels, you can identify any fluctuations and make adjustments to your lifestyle or treatment plan as needed. Regular monitoring provides valuable insights into your body's response to different foods, exercise, and stress.
Managing Stress and Mental Well-being
Stress management and taking care of your mental well-being are crucial for long-term success in living with diabetes Type 2 remission. Chronic stress can negatively impact blood sugar levels and overall health. Engaging in stress-reducing activities such as meditation, deep breathing exercises, or hobbies that you enjoy can help improve your mental well-being. Additionally, seeking support from healthcare professionals, joining support groups, or talking to loved ones about your journey can provide emotional support and encouragement.
By following these long-term strategies, individuals with diabetes Type 2 remission can maintain a healthy and fulfilling life. It's important to remember that although remission is possible, it requires continued commitment to a healthy lifestyle and regular monitoring of blood sugar levels.
Frequently Asked Questions about Diabetes Type 2 - How to Permanently Cure Diabetes Type 2: Effective Strategies to Achieve Remission

Have questions about managing and reversing Diabetes Type 2? We've got answers. Check out the frequently asked questions below for essential insights into diabetes remission and long-term strategies for a healthier life.
Is it possible to permanently cure Diabetes Type 2?
While no definitive cure exists for Diabetes Type 2, lifestyle changes can effectively manage and put it into remission. By adopting healthy habits such as weight loss, regular exercise, and a balanced diet, many individuals can achieve normal blood sugar levels without the need for medication.
How can weight loss help in remission?
Weight loss plays a crucial role in achieving remission from Diabetes Type 2. Shedding excess pounds reduces insulin resistance, improves blood sugar control, and allows the body to utilize insulin more effectively. We recommend working with healthcare professionals to develop a personalized weight loss plan that includes nutrition guidance and physical activity.
Are there natural therapies for diabetes reversal?
Although there is no natural therapy that can cure Diabetes Type 2, certain lifestyle changes can help manage the condition. Implementing stress-reducing techniques, such as mindfulness and relaxation exercises, can support overall well-being and contribute to better diabetes control.
What role does medication play in remission?
Medication can be an important component of managing Diabetes Type 2, especially for individuals who have difficulty achieving blood sugar control through lifestyle changes alone. Various oral medications and injectable insulin can help regulate blood sugar levels, thereby supporting the quest for remission. Consult with a healthcare provider to determine the most suitable medication regimen.
Can exercise alone reverse Diabetes Type 2?
Exercise, when combined with dietary modifications, is a highly effective approach to achieving normal blood sugar levels in Diabetes Type 2. Engaging in regular physical activity improves insulin sensitivity, aids in weight management, and enhances overall cardiovascular health. You should consult with a healthcare professional to develop an exercise plan tailored to individual needs.
Is bariatric surgery a recommended option?
Obese individuals with Diabetes Type 2 may consider bariatric surgery, such as gastric bypass or gastric sleeve, as an option for weight loss and diabetes reversal. This surgical intervention can significantly improve blood sugar control and metabolic health. However, it is crucial to discuss the potential risks and benefits with a healthcare provider.
How important is early diagnosis and intervention?
Early diagnosis and intervention are paramount in managing Diabetes Type 2 effectively. Detecting the condition early allows for timely implementation of lifestyle changes, leading to better blood sugar control and increased chances of achieving remission. Regular screenings and routine check-ups are key to catching diabetes early.
Is achieving remission without medication possible?
In some cases, significant lifestyle changes can achieve remission from Diabetes Type 2 without medication. Weight loss, adopting a healthy diet, and engaging in regular exercise can help normalize blood sugar levels. It is essential to work closely with healthcare professionals to monitor progress and adjust the treatment plan, if necessary.
What are the potential complications of Diabetes Type 2?
Diabetes Type 2 can lead to several complications if left unmanaged. These include cardiovascular problems, nerve damage, kidney disease, eye issues, and an increased risk of infections. However, implementing lifestyle changes and controlling blood sugar levels can significantly reduce the risk of developing these complications.
Where can I find additional support and resources?
Plenty of support and resources are available to those living with Diabetes Type 2. Consider reaching out to healthcare professionals, diabetes education programs, and support groups for guidance, information, and practical tools to manage the condition effectively.
Remember, the journey to diabetes remission is unique for each individual. By understanding the condition, prioritizing lifestyle changes, and seeking the appropriate support, you can take proactive steps towards a healthier, more balanced life.



